Interstitial Cystitis: How This Bladder Disorder Is Linked to Leaky Gut Syndrome
Interstitial cystitis, also known as bladder pain syndrome, is a chronic condition that affects the bladder wall. It causes discomfort, pressure, tenderness, or pain in the bladder, lower abdomen, and pelvic area. The symptoms can be constant or come and go, making it a challenging condition to manage.
Interstitial cystitis is an autoimmune disease where the immune system mistakenly attacks healthy cells and tissues in the body. In the case of interstitial cystitis, the immune system may be attacking the bladder wall, leading to inflammation and pain.
Interstitial cystitis affects women more frequently than men, and the symptoms usually start in their 30s or 40s. There are certain factors that can increase the risk of developing this condition, such as a previous pelvic surgery, chronic urinary tract infections, and a family history of interstitial cystitis.
Interstitial Cystitis Symptoms
Some common symptoms include:
- Urinary Frequency: Individuals with IC often experience an increased frequency of urination. This means they feel the need to urinate more often than usual, even if only small amounts of urine are passed.
- Urgency: IC can cause a strong, sudden urge to urinate that may be difficult to control. This urgency can contribute to anxiety and discomfort.
- Pain: Pain is a hallmark symptom of IC. It can range from mild discomfort to severe pain in the bladder, pelvis, and lower abdomen. The pain may be intermittent or constant and can be described as aching, burning, or pressure.
- Painful Intercourse: Many individuals with IC experience pain or discomfort during sexual intercourse, a condition known as dyspareunia.
- Pelvic Pain: In addition to bladder-related pain, IC can cause generalized pelvic pain that may extend to the lower back and groin.
- Nocturia: Nocturia refers to the need to urinate multiple times during the night, which disrupts sleep patterns.
- Painful Urination (Dysuria): People with IC may experience pain or discomfort while urinating, similar to the sensation of a urinary tract infection.
- Flare-ups: IC symptoms can vary over time. Some individuals experience periods of symptom exacerbation, known as flare-ups, followed by periods of remission with milder symptoms.
- Pressure or Discomfort: A sensation of pressure or discomfort in the bladder area, even when the bladder is not full, is another common symptom.
- Emotional Impact: The chronic nature of IC and the associated pain and discomfort can lead to emotional distress, including anxiety and depression.
Treatments
There are several treatments available in order to minimize and treat Interstitial Cystitis symptoms.
Lifestyle Modifications:
- Bladder Training: Gradually extending the time between urinations can help improve bladder capacity and reduce urgency.
- Stress Management: Manage your stress levels and practice relaxation techniques. Stress can activate your sympathetic nervous system (the fight-or-flight response) and cause a surge of adrenaline and cortisol. This can exacerbate your symptoms and damage your nerves over time.
- Get enough sleep and follow a regular sleep schedule. Sleep is essential for repairing your body and regulating your hormones. Lack of sleep can impair your cognitive function, mood, metabolism, and immune system.
- Exercise moderately and regularly but avoid overexertion or extreme temperatures. Exercise can improve your cardiovascular health, muscle tone, blood flow, and mood. However, too much exercise or exposure to heat or cold can trigger your symptoms and cause a drop or spike in your blood pressure or heart rate.
Dietary Changes:
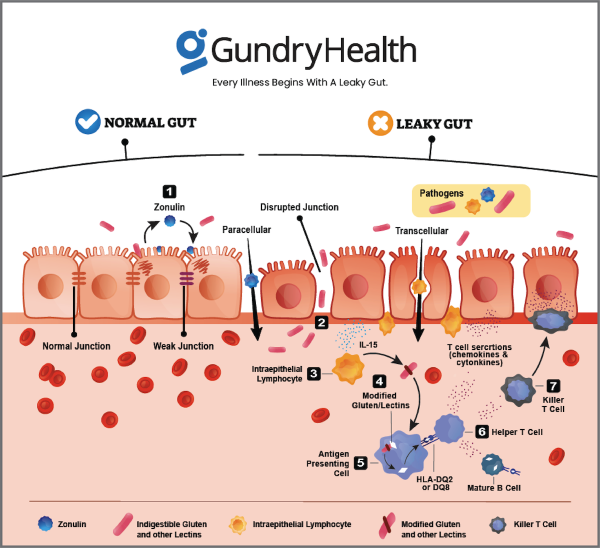
- Avoiding Trigger Foods: Eat a balanced diet that is rich in plant-based foods, healthy fats, and lean proteins. Avoid foods that are high in sugar, refined carbs, lectins, gluten, dairy, soy, corn, and nightshades. Eating these foods may trigger a condition called Leaky Gut Syndrome, which in turn can complicate the IC treatments and may lead to even more autoimmune conditions. These foods can trigger inflammation, disrupt your gut microbiome, and impair your immune system2 Keeping a food diary can help identify personal triggers.
- Hydration: Drinking plenty of water and staying hydrated is important, but it’s best to avoid drinking large amounts of fluid at once.
Furthermore, many people with interstitial cystitis resort to medications or procedures to manage their symptoms or improve their bladder condition. However, these treatments can also have negative effects on your gut health. For example,
- Antibiotics can reduce infection but can also kill the good bacteria in your gut.
- Anti-inflammatory drugs can reduce pain but can also damage the gut lining or cause ulcers.
- Bladder instillation can deliver medication directly into the bladder but can also introduce infections into the urinary tract.
- Bladder distension can stretch the bladder wall but can also cause trauma to the bladder or intestines.
How To Diagnose Interstitial Cystitis
Diagnosis can be complex and the symptoms can vary widely. IC is often diagnosed by excluding other potential causes of similar symptoms through a combination of the below listed methods.
- Medical History and Symptoms: Your healthcare provider will begin by discussing your medical history and the symptoms you are experiencing. Be prepared to provide details about the type and duration of pain, urinary frequency, urgency, and any other discomfort you’re feeling.
- Physical Examination: A physical examination, including a pelvic examination, may be performed to assess your pelvic and bladder area for signs of tenderness, inflammation, or other abnormalities.
- Diagnostic Criteria: The American Urological Association (AUA) and the International Continence Society (ICS) have established criteria called the “AUA/ICSI Criteria” that help guide the diagnosis of IC. These criteria include specific symptom patterns, duration of symptoms, and exclusion of other possible causes.
- Urine Tests: Urinalysis and urine cultures are conducted to rule out infections and other urinary tract disorders that can mimic IC symptoms.
- Cystoscopy: Cystoscopy is a procedure in which a thin tube with a camera (cystoscope) is inserted into the urethra and guided into the bladder. This allows the healthcare provider to directly visualize the bladder lining for signs of inflammation, bleeding, or other abnormalities.
- Biopsy: In some cases, during cystoscopy, a small tissue sample (biopsy) of the bladder lining may be taken to rule out other conditions that can cause similar symptoms, such as bladder cancer.
- Potassium Sensitivity Test: This test involves instilling a solution containing potassium into the bladder to see if it causes symptoms similar to IC. However, this test is not widely used and is not considered definitive for IC diagnosis.
- Urodynamic Testing: Urodynamic tests evaluate how well the bladder and urethra store and release urine. While not specific to IC, these tests can help assess bladder function and rule out other bladder disorders.
How To Prevent or Heal Interstitial Cystitis and Leaky Gut Syndrome with Diet and Lifestyle Changes at Gundry Health?
Living with interstitial cystitis can be challenging, both physically and emotionally. It can affect a person’s quality of life, leading to anxiety, depression, and social isolation. However, there are resources and support groups available to help people cope with this condition. The Interstitial Cystitis Association, for example, provides information, support, and advocacy for people affected by interstitial cystitis.
While some forms of interstitial cystitis and leaky gut syndrome are not preventable, you can still take steps to improve your overall health and reduce your risk of complications. Some of the best ways to do so are:
- Eat a balanced diet that is rich in plant-based foods, healthy fats, and lean proteins. Avoid foods that are high in sugar, refined carbs, lectins, gluten, dairy, soy, corn, and nightshades. These foods can trigger inflammation, disrupt your gut microbiome, and impair your immune system2
- Drink plenty of water and stay hydrated throughout the day. Dehydration can worsen your symptoms and affect your blood volume and pressure.
- Avoid alcohol, caffeine, nicotine, and drugs that can interfere with your bladder function. These substances can cause dehydration, increase your heart rate and blood pressure, and affect your mood and sleep quality.
- Manage your stress levels and practice relaxation techniques. Stress can activate your sympathetic nervous system (the fight-or-flight response) and cause a surge of adrenaline and cortisol. This can exacerbate your symptoms and damage your nerves over time.
- Get enough sleep and follow a regular sleep schedule. Sleep is essential for repairing your body and regulating your hormones. Lack of sleep can impair your cognitive function, mood, metabolism, and immune system.
- Exercise moderately and regularly but avoid overexertion or extreme temperatures. Exercise can improve your cardiovascular health, muscle tone, blood flow, and mood. However, too much exercise or exposure to heat or cold can trigger your symptoms and cause a drop or spike in your blood pressure or heart rate.
Recent findings suggest that interstitial cystitis affects up to 6.5% of women in the United States, making it more common than previously thought. Researchers are also exploring new treatments and potential causes of this condition. For example, some studies have suggested that a lack of certain gut bacteria may play a role in the development of interstitial cystitis.
At Gundry Health, we offer a holistic approach to clinical care that addresses the root causes of interstitial cystitis and leaky gut syndrome. We use a combination of lab data (blood tests), provider treatment (medications), dietary changes (lectin-free diet), supplements (probiotics), lifestyle modification (stress management), alternative therapies (acupuncture), procedures (bladder instillation), surgery (if needed), as well as education (books) to help you heal your gut and improve your overall health. By following our protocol, you can prevent or heal interstitial cystitis and leaky gut syndrome and reduce the risk of autoimmune disease.
In conclusion, interstitial cystitis is a chronic condition that affects the bladder wall, causing pain, discomfort, and other symptoms. It is essential to work with your doctor to manage your symptoms effectively and improve your quality of life. There are resources and support groups available to help people affected by interstitial cystitis, and researchers continue to explore new treatments and potential causes of this condition.
Get personalized care and recommendations for interstitial cystitis from Dr Gundry-Approved program
If you’re looking for more guidance about interstitial cystitis disease than this short list of recommendations, Dr. Gundry’s unique health program is now available to you (without needing an appointment at one of Dr. Gundry’s two, waitlist-only West Coast clinics).
Thanks to the pioneering work of Dr. Gundry and his team at Gundry Health, patient care team trained in Dr. Gundry’s unique holistic methods are now available to help you craft your own personalized interstitial cystitis program.
It’s easy to get started.
Simply click the link below to get more information about personalized interstitial cystitis treatment plan options, so you can get expert analysis, diagnostic care, and a plan for tackling interstitial cystitis, arthritis, or other autoimmune diseases.
Each patient care team member at Gundry Health is Board Certified and trained in Dr. Gundry’s renowned approach to functional medicine and care.
Get your personal lab data and talk to a U.S. licensed doctor. Click Here.
If you have any questions or concerns about interstitial cystitis or leaky gut syndrome, please contact us at Gundry Health to schedule an appointment with one of our qualified health professionals. You can also visit our website for more information and resources
1: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5605935/
2: https://gundrymd.com/lectin-free-diet/