Leaky Gut: What Is It and Is There a Cure?
Dr. Steven Gundry Says Yes.
Learn more about the signs of leaky gut, how it is at the root of most autoimmune diseases, and how it’s treated.
What is leaky gut syndrome?
It may surprise you to hear that disease begins in your gut, just as the father of modern medicine, Hippocrates, said over 2,400 years ago.
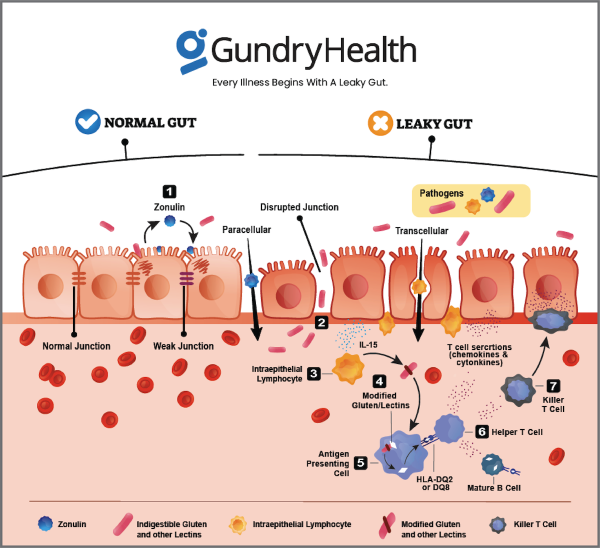
That’s because the immune cells along your gut lining play an important role in keeping your gut wall strong. They decide what can leave the GI tract and what must stay contained.
When everything is working well, nothing gets through this strong gut barrier except what’s supposed to. However, when this barrier gets worn down (more on that below) and develops more and more microscopic holes, it allows other compounds to “leak” through, causing your health to suffer.
Making Hard, Easy.
This is the condition known as “leaky gut syndrome.”
What are the signs of a leaky gut?
Leaky gut can be difficult to diagnose. That’s because many symptoms of leaky gut – like painful indigestion, diarrhea, gas and bloating from meals, brain fog, low energy and even common skin conditions like rashes – are often considered “normal” by many doctors.
Over time, however, persistent gastrointestinal upset, constant gas and bloating, and chronic low energy can all be signs of a leaky gut. And if left untreated, leaky gut can eventually lead to the development of autoimmune diseases like Crohn’s disease, ulcerative colitis, hypothyroidism, lupus, multiple sclerosis, rheumatoid arthritis, psoriasis, and more.
Intestinal permeability – what is it?
To understand exactly how leaky gut works on a scientific level, you need to first understand more about how your gut wall functions. Your intestines are lined with a single layer of mucosal cells (called enterocytes), which are locked tightly together to prevent material from entering or escaping. Though this intestinal layer is only one cell thick, its surface area is equivalent to the size of a tennis court.
The immune cells (specialized white blood cells) positioned along and interspersed within that lining play an important role in maintaining the integrity of the wall. In fact, about 70-80 percent of all your immune cells are concentrated along the lining of your gut.1 These immune cells are responsible for deciding what can leave the GI tract and what must stay contained.
Your stomach acids, enzymes, and beneficial gut bacteria break down the food you eat into individual components: amino acids, fatty acids, and sugar molecules. Your mucosal cells then bite off a single molecule of these digested amino acids, fatty acids, and sugars, pass it through the body of the cell, and release it into your portal vein or lymph system.
When all is working well, everything besides these single molecules remains outside the intestinal barrier, where it belongs.If your mucosal cells are lined up tightly side by side, your gut lining will help keep everything except single molecules of digested amino acids, fatty acids, and sugar on the other side.
However, when your gut wall gets worn down and becomes rife with microscopic holes, it will allow other compounds to “leak” through, and your health will begin to suffer. This is the definition of “leaky gut syndrome,” also known as intestinal permeability.
What causes intestinal permeability (aka leaky gut syndrome)?
Each of us has a community of bacteria living inside our gut called the microbiome. And your microbiome is made up of both “good” and “bad” bacteria. These so-called “good bacteria” have three main jobs: help you digest your food, manufacture important nutrients, and tell your immune system and brain what’s going on inside your gut.
However, over the past 50-100 years, humans in the industrialized world have begun eating more and more of the wrong foods – foods that their gut bacteria (especially their beneficial gut bacteria or “gut buddies” as Dr. Gundry calls them) have trouble digesting. One particularly harmful food, sugar, acts like fuel for the harmful bacteria living inside of our gut.
According to Dr. Steven Gundry, a cardiothoracic surgeon and New York Times best-selling author, another cause of intestinal permeability is lectins. Lectins are a type of plant protein that helps defend plants from getting eaten. These plant proteins can force apart the tight junctions between the cells lining your intestinal walls by attaching themselves to your gut lining.
In other words, lectin-containing nightshade plants like tomatoes, cucumbers, potatoes, eggplants, and even goji berries can actually cause intestinal permeability – especially in people who already have a weakened immune system or an unbalanced gut microbiome.
Not only that, but environmental factors can also play a role in destabilizing the gut microbiome and causing intestinal permeability. For example, the common weed killer glyphosate (with over 280 million pounds applied annually to nearly 300 million acres of farmland in the U.S. alone2) has now been shown to affect the human microbiome.3 Additionally, common over-the-counter medications called non-steroidal anti-inflammatories (NSAIDs) can affect both gut permeability and the composition of the microbiome.4-5
Leaky gut and autoimmune diseases – a surprising connection
When the wrong molecules or even bacteria get across the border of your gut wall, your immune system kicks into high gear. Normally, this is really important since your immune system can call in “reinforcements” – inflammatory hormones called cytokines.
These cytokines can save your life from a bacterial infection and help you heal when you have an injury.
The problem starts when your immune system starts responding to every little thing – including environmental triggers or food allergies. Think of it like an overactive security alarm system. You’re grateful when it alerts you to the presence of a thief, but you’re annoyed when it goes off every time a fly enters your home.
That’s exactly what happens when you have a leaky gut. Your immune system begins responding to everything that gets through your porous gut wall. This leads to chronic inflammation.
Now, what does this all have to do with common autoimmune diseases like arthritis, hypothyroidism, and irritable bowel disease? Well, the zonulin gene sits on a certain chromosome linked to many autoimmune diseases, certain types of cancer, and diseases of the nervous system like multiple sclerosis. In other words, there’s a clear connection between a leaky gut and the formation of autoimmune diseases.
So while genetics and your environment can play a role in whether you develop autoimmune diseases, a leaky gut is the crucial third ingredient. This is why it’s so important to keep your gut wall strong. And unlike your genetics, and often unlike your environment, you can fix a leaky gut with the foods you eat and more importantly, the foods you don’t eat.
How is leaky gut diagnosed?
In his private practice, Dr. Gundry always begins with blood work. He looks for specific markers of inflammation and leaky gut, before asking the patient a battery of questions about symptoms, diet, and lifestyle. Once he’s made his diagnosis, Dr. Gundry works with his patients to craft a personalized care and lifestyle routine.
The cure for leaky gut
If you suspect you may have a leaky gut, there are some steps you can take at home right now.
First, eat more prebiotic fiber. Prebiotics are the food your beneficial gut bacteria love to eat. And they’re particularly good for you precisely because you can’t digest them. Prebiotics pass through your stomach and into your gut, where your “good” bacteria can digest them.
Prebiotic-rich vegetables include artichokes, leeks, okra, jicama, broccoli, Jerusalem artichokes, cauliflower, radicchio, and chicory. You can also find prebiotics in mushrooms and some nuts. If this isn’t possible, find a sugar-free fiber supplement.
Second, you may also want to cut lectin-containing foods from your diets. These include foods like oats, quinoa, brown rice, barley, rye, and whole wheat – along with nightshades like tomatoes, potatoes, and peppers. In general, you can begin to follow Dr. Gundry’s YES and NO foods list to help reduce inflammation.
However, please keep in mind that nutrition is highly personalized. What’s right for one person may not be right for someone else. So while these recommendations are generalizable, following these suggestions may not solve your leaky gut.
That’s why it’s important to speak with a certified expert who can give you more personalized diet and lifestyle recommendations.
Get your own personalized leaky gut care and recommendations from Dr Gundry-approved care coordinators
If you’re looking for more guidance than these simple recommendations for your leaky gut, Dr. Gundry’s unique health program is now available to you (without needing an appointment at one of Dr. Gundry’s two, waitlist-only West Coast clinics).
Thanks to the pioneering work of Dr. Gundry and his team at Gundry Health, care coordinators trained in Dr. Gundry’s unique holistic methods are now available to help you craft your own personalized leaky gut program.
–
1 Wiertsema SP, van Bergenhenegouwen J, Garssen J, Knippels LMJ. The Interplay between the Gut Microbiome and the Immune System in the Context of Infectious Diseases throughout Life and the Role of Nutrition in Optimizing Treatment Strategies. Nutrients. 2021;13(3):886. Published 2021 Mar 9. doi:10.3390/nu13030886
2 U.S. Environmental Protection Agency. Glyphosate: Response to Comments, Usage, and Benefits. April 18, 2019. Accessed June 18, 2022. https://www.epa.gov/sites/default/files/2019-04/documents/glyphosate-response-comments-usage-benefits-final.pdf
3 Leino L, Tall T, Helander M, et al. Classification of the glyphosate target enzyme (5-enolpyruvylshikimate-3-phosphate synthase) for assessing sensitivity of organisms to the herbicide. J Hazard Mater. 2021;408:124556. doi:10.1016/j.jhazmat.2020.124556
4 Bjarnason I, Takeuchi K. Intestinal permeability in the pathogenesis of NSAID-induced enteropathy. J Gastroenterol. 2009;44 Suppl 19:23-29. doi:10.1007/s00535-008-2266-6
5 Rogers MAM, Aronoff DM. The influence of non-steroidal anti-inflammatory drugs on the gut microbiome. Clin Microbiol Infect. 2016;22(2):178.e1-178.e9. doi:10.1016/j.cmi.2015.10.003