A Cure for Sarcoidosis?
Discover Common Sarcoidosis Symptoms and Dr. Steven Gundry’s Recommended Sarcoidosis Treatment
Find out what causes sarcoidosis, how dangerous sarcoidosis is, and whether there’s really a cure for sarcoidosis.
What is sarcoidosis?
Sarcoidosis is a rare disease in which tiny clumps of inflammatory cells, called granulomas, collect on various organs of the body. This can often lead to inflammation on the organs themselves, which can lead to further health complications.
While sarcoidosis most commonly affects the lungs (it’s estimated that around 90% of sarcoidosis cases involve the lungs), it can also affect other organs, including the heart, brain, lymph nodes, skin, and more. So it’s important that doctors thoroughly examine their patients if they suspect a case of sarcoidosis.
Symptoms of sarcoidosis: is it a disease of the lungs?
Some cases of sarcoidosis may not have any symptoms at all, making diagnosis and treatment more difficult. This is why some doctors only discover the disease when examining a patient’s chest x-ray. (This may also be why some cases are not caught until the patients are well into middle age.)
When symptoms do appear, however, they can appear gradually. Common initial symptoms of sarcoidosis include:
- Fatigue
- Weight loss
- Swollen lymph nodes
- Pain and swelling in joints
And since around 90% of sarcoidosis cases involve the lungs, you should also be on the lookout for the following symptoms:
- Chest pain (particularly around your breastbone)
- Wheezing
- Persistent dry cough
- Shortness of breath
Sarcoidosis can also cause skin problems, as well. Symptoms of sarcoidosis of the skin include:
- Skin rashes (look out for red or reddish-purple bumps – usually on the shin or ankles – that are also warm and tender to the touch)
- Skin sores (these often appear on the nose, cheeks, and ears)
- Areas of the skin that appear lighter or darker in color than the skin around it
- Raised scars or raised skin around a tattoo
Sarcoidosis can also affect other organs of the body, including your heart, eyes, and nervous system. Look out for some of these symptoms if you suspect your may have sarcoidosis of organs other than your lungs:
- Blurred vision
- Eye pain
- Burning, itching, or dry eyes
- Fainting
- Irregular heart beats
- Rapid or fluttering heart beat
- Seizures
- Hearing loss
- Headaches
What causes sarcoidosis?
Sarcoidosis is technically an inflammatory disease. And while it’s believed to be caused by the body’s immune response to an inflammatory trigger, there’s still some academic debate over whether sarcoidosis might actually be an autoimmune disease.
However, many experts now believe sarcoidosis is caused by the body’s immune system responding to some foreign substance. This could be an infectious agent, a chemical, or some other kind of allergen or trigger.
And according to Dr. Steven Gundry, the former head of cardiothoracic surgery at Loma Linda University and founder of the Centers for Restorative Medicine, a major cause of sarcoidosis may also include the common condition known as leaky gut (more on this below).
How does sarcoidosis progress?
Progression of the disease can often be divided into three phases:
- Inflammation on a cellular level.
- Tiny clusters of these inflamed cells – called granulomas – start forming. (Think of granulomas like floating defenses your body uses to isolate the cause of your inflammation.)
- Scarring of tissues or organs occurs. Too much scarring of a vital organ can occasionally lead to death.
Do I have sarcoidosis?
Some groups of people seem more likely to get sarcoidosis than others. For example, Irish immigrants in London are 3 times more likely to develop sarcoidosis than native Londoners.
In the United States, sarcoidosis is more common among the African-American population (anywhere from a 4 to 17 times greater risk than the Caucasian population). And the risk that you might get sarcoidosis increases 5 times if a first- or second-degree relative has had the disease.
Surprisingly, sarcoidosis is most common among young people ages 20-40 (although it can still affect the elderly). According to the Illinois Department of Public Health, the greatest risk in the U.S. population is among young African-American adults (especially women), or young people of Scandinavian, Irish, German, or Puerto Rican descent. While white women are just as likely as white men to get sarcoidosis, African-American women get sarcoidosis twice as often as African-American men.
Is sarcoidosis dangerous?
While many instances of sarcoidosis come and go without any treatment needed, some cases are more serious – and can even be fatal. In fact, the seriousness of sarcoidosis is entirely dependent on 4 factors:
- How long the disease has been affecting you.
- Where the granulomas are forming (e.g. your lungs, your heart, your skin, etc.).
- How much tissue has been affected by the granulomas.
- Whether granulomas are still forming or have developed into scar tissue.
When scarring becomes extensive in an important organ – like your lungs or heart – it can be fatal, causing heart attacks or serious long-term damage.
How is sarcoidosis diagnosed and treated?
Because of its rarity, sarcoidosis can remain undetected for months or even years. And because it most commonly affects the lungs, sarcoidosis is sometimes misdiagnosed as pulmonary fibrosis (a lung disease where lung tissue becomes damaged and scarred).
Doctors will normally use some of the following tools to try and diagnose a case of sarcoidosis:
- Chest x-ray
- CT scan
- Pulmonary function test
- Blood test
- Bronchoscopy
- Bronchoalveolar lavage
- Lung biopsy
However, because not all forms of sarcoidosis affect only the lungs, it’s important to pay attention to your own symptoms and speak candidly with your doctor or specialist.
Once sarcoidosis has been diagnosed, though, treatment options are often limited. That’s because there’s no cure for sarcoidosis – only different forms of treatment of its symptoms.Typically, patients are prescribed various medications to suppress the immune system and reduce inflammation. Examples include:
- Corticosteroids – steroids like prednisone are the most commonly prescribed treatment for sarcoidosis. Side effects typically include mood swings, weight gain, high blood pressure, upset stomach, and excess fluid retention among other long-term effects.
- Antimalarial drugs – Surprisingly, medications like hydroxychloroquine can help with symptoms of sarcoidosis affecting the skin and joints.
- Disease modifying antirheumatic drugs (DMARDs) – these are prescription drugs that suppress the immune system to slow the progression of sarcoidosis and reduce symptoms. Side effects include diarrhea, rashes, stomach upset, and in some cases, birth defects.
Is there a cure for sarcoidosis?
Unfortunately, there is no cure for sarcoidosis. That means most doctors will only look to manage your symptoms and hope any damage to your organs or tissues reduces over time.
However, celebrated cardiologist and New York Times best-selling author Dr. Steven Gundry has developed a comprehensive plan to help his patients dealing with autoimmune and inflammatory diseases like sarcoidosis.
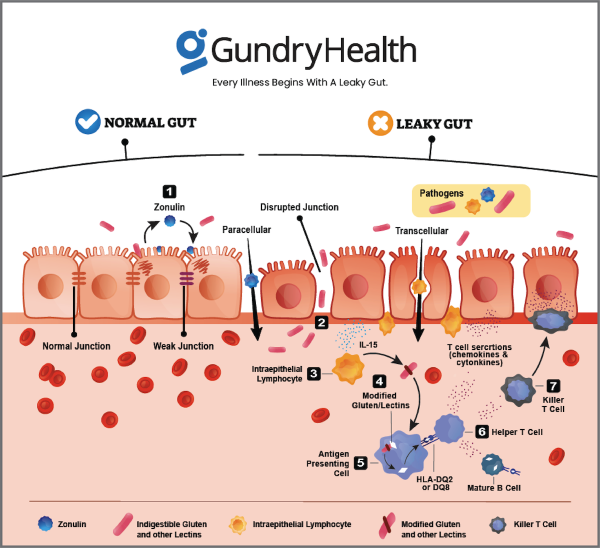
According to Dr. Gundry, an overactive immune system often signals an imbalance in your microbiome (all the bacteria and microorganisms that live inside your gut). This condition is sometimes called leaky gut.
You see, the immune cells along your gut lining play an important role in keeping your gut wall strong. They decide what can leave the GI tract and what must stay contained.
When everything is working well, nothing gets through this strong gut barrier except what’s supposed to. However, when this barrier gets worn down (more on that below) and develops more and more microscopic holes, it allows other compounds to “leak” through, causing your health to suffer.
So when the wrong molecules or even bacteria get across the border of your gut wall, your immune system kicks into high gear. Normally, this is really important since your immune system can call in “reinforcements” – inflammatory hormones called cytokines. These cytokines can save your life from a bacterial infection and help you heal when you have an injury.
The problem starts when your immune system starts responding to every little thing. Think of it like an overactive security alarm system. You’re grateful when it alerts you to the presence of a thief, but you’re annoyed when it goes off every time a fly enters your home.
That’s exactly what happens when you have a leaky gut. Your immune system begins responding to everything that gets through your porous gut wall. This leads to chronic inflammation – including the kind of inflammation on your skin that causes sarcoidosis.
In other words, a leaky gut – which is often caused by environmental triggers like certain foods, chemicals, or stress – leads directly to sarcoidosis.
Treatment for sarcoidosis – the link to leaky gut
In order to start reducing your sarcoidosis symptoms, you need to understand what causes a leaky gut in the first place. When you take care of the problem at the source, you can dramatically lessen the frequency and severity of your eczema.
Imagine your body is a fortress. You need a wall to protect yourself. That’s your gut wall. Immune cells are the soldiers there to protect your fortress. Their job is to detect friend from foe. And when they fight for you, they cause collateral damage. We call that collateral damage inflammation.
However, your protective walls aren’t sealed shut. All along the wall are tiny doors. And while these doors are closed most of the time, sometimes they need to open to allow food or friends to come in.
So imagine what would happen if those doors were always open. It would be much harder for your soldiers to defend the fortress (your body). Now, there is a molecule (called zonulin) inside your body that makes these “doors” in your gut wall open or close. And there are certain environmental triggers that make your cells produce zonulin.
One such trigger is a type of protein called a lectin. Plants produce lectins as a defense against being eaten. In fact, lectins are so powerful they can even paralyze the bugs that eat them.
Of course, you’re a lot bigger and stronger than a little bug. And you have your own defense mechanisms, like mucus, which can bind to lectin proteins and make them harmless as you digest them.
However, as humans have consumed more and more lectin-rich foods (like tomatoes, potatoes, beans, and most grains) our natural defenses against these pesky proteins have begun to weaken.
And when lectins make it through to your GI tract, they can cause all kinds of problems. For one, they bind with receptors along the gut lining to produce zonulin. As explained above, zonulin then breaks the tight junctions holding together your gut wall. This creates spaces between the cells for “foreign invaders” (like harmful bacteria) to get through and get to other parts of your body.
The result? Inflammation.
This is why reducing lectin consumption is a major part of Dr. Gundry’s health program. (Click HERE to find a complete list of lectin-containing foods you should avoid if you’re suffering from eczema.)
Dr. Gundry has helped thousands of his patients – and many more people through his best-selling books such as The Plant Paradox – to get rid of autoimmune and inflammatory diseases like sarcoidosis. He’s done this by utilizing the latest blood and laboratory tests and combining these test results with a comprehensive personalized diet and nutrition program.