Rheumatoid Arthritis vs. Lupus: Understanding the Differences
Autoimmunity affects everyone differently, and when comparing RA and lupus, many wonder which is worse. Both are common autoimmune diseases, with an estimated 1.5 million Americans suffering from lupus.
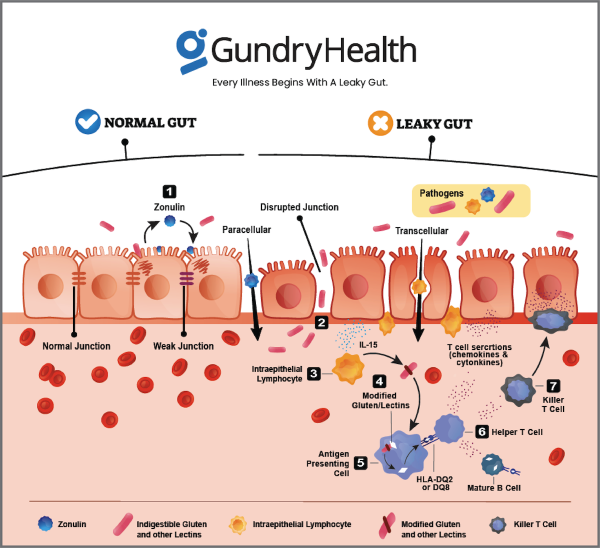
To understand the differences between the two, it’s important to grasp the fundamentals of each disease. While they share common symptoms, such as joint pain and inflammation, RA primarily affects the joints and surrounding tissue, while lupus can affect multiple organs and systems in the body. At Gundry Health, we work directly with individuals with autoimmune diseases to help them identify and remove their unique triggers, reducing symptoms and improving their quality of life.
Understanding Rheumatoid Arthritis: Causes, Symptoms, and Prevalence
Rheumatoid arthritis (RA) is an autoimmune disease that causes chronic inflammation of joint linings, leading to joint damage and chronic pain. The disease can also cause bone erosion, joint deformity, and damage to other organs such as the lungs, heart, skin, eyes, kidneys, and blood vessels. RA often starts in small joints in the hands and feet, and can spread to other joints such as wrists, elbows, shoulders, knees, and hips as the disease progresses.
RA affects over 1.3 million people in the US and is the most common type of autoimmune arthritis. The disease predominantly affects women, with 75% of people with RA being female. Understanding the causes, symptoms, and prevalence of RA is crucial for early detection, proper treatment, and management of the disease.
Lupus: Understanding the Symptoms, Risk Factors, and Treatment
Lupus is a chronic autoimmune disease that causes inflammation and pain, affecting different parts of the body such as the skin, kidneys, brain, blood cells, and heart. Lupus is most common among women, accounting for 90% of all cases.
Here are some risk factors associated with lupus:
- Genetics
- Environment
- Virus and bacteria
- Diet
- Medications (drug-induced lupus)
- Female hormones like estrogen
- Sunlight
- A combination of the above factors
Although many people experience mild forms of lupus with periodic symptom flare-ups, severe cases can result in debilitating symptoms. Early diagnosis and treatment can help to reduce the severity of symptoms and improve overall quality of life.
5 Similarities Between Lupus and Rheumatoid Arthritis Symptoms
Lupus and rheumatoid arthritis (RA) are both autoimmune diseases, characterized by joint inflammation and other symptoms. Here are five similarities between the two conditions:
- Both diseases can be caused by genetic and environmental factors.
- Lupus and RA can both affect multiple joints, causing pain, swelling, inflammation, and stiffness.
- Fatigue is a common symptom of both lupus and RA, often accompanied by weakness.
- Women are more likely to develop both lupus and RA than men.
- Both diseases involve periods of flare-ups, where symptoms worsen, followed by periods of remission. While there is no cure for either condition, treatment is available to manage symptoms and improve quality of life.
Personalized treatment is essential for both lupus and RA, including an individualized diet. However, navigating these treatments can be challenging without proper guidance.
Differences Between Rheumatoid Arthritis and Lupus
Rheumatoid arthritis (RA) and lupus are both autoimmune diseases that affect the joints, but they differ in several ways:
- RA joint pain is worse in the morning, while lupus pain is more consistent.
- RA joint pain can lead to joint deformities, but joint pain and stiffness with lupus do not cause deformities.
- Lupus patients are sensitive to the sun, which can trigger a butterfly-shaped red or brown skin rash over the cheeks and nose. Photosensitivity is not common in RA.
- Lupus attacks multiple tissues and organs of the body, including the kidneys, making it a leading cause of death in young women aged 19-49 in the US. RA targets the lining of the joints and rarely has organ involvement in disease progression.
- Lupus can have a rash associated with it, whereas RA may have redness only in the specific joints that are inflamed.
Individualized treatment for both diseases can help improve quality of life and reduce symptoms. It can be helpful to identify triggers for flares as both diseases involve the body attacking itself as if infected by a virus or bacteria.
Is RA Worse Than Lupus? Understanding the Differences and Similarities
While both RA and lupus are autoimmune diseases, neither is worse than the other. Each condition is unique and requires individualized treatment. Lupus can be more deadly than RA, making effective treatment crucial. However, RA already has effective treatments available. Understanding the differences and similarities between the two conditions is key to managing symptoms and improving quality of life.
Can Gundry Health Help Manage Lupus and RA Symptoms?
At Gundry Health, we provide a personalized treatment approach for each patient, including those with lupus and RA. Our care coordinators work with patients to track their symptoms and identify potential triggers for flare-ups versus remission.
We understand that certain foods and environmental factors can increase inflammation and aggravate symptoms. Through our experience in supporting patients with autoimmunity, we have found that triggers can vary between individuals and diseases.
Gundry Health program provides nutritional support, stress management techniques, and supplement recommendations to help patients manage their symptoms and improve overall health.
If you’re interested in exploring how Gundry Health can help manage your lupus or RA symptoms, get started by scheduling a consultation with one of our care coordinators.