Raynaud’s Phenomenon: Understanding and Managing the Condition with Gundry Health
Raynaud’s phenomenon, also known as Raynaud’s syndrome or Raynaud’s disease, is a medical condition that affects the blood vessels, particularly the small arteries that supply blood to the extremities, such as the fingers and toes. This condition is characterized by episodes of reduced blood flow to these extremities, leading to color changes in the skin and symptoms like numbness, tingling, and pain.
Understanding Raynaud’s Phenomenon
Raynaud’s phenomenon is a condition characterized by small blood vessels in the fingers or toes spasming in response to cold or stress. This narrows the vessels dramatically, causing the skin to turn blue, feel cold and numb, and then redden upon warming.
Causes, Symptoms, and Treatment
The exact cause of Raynaud’s is unknown, but it’s thought to involve improper nerve control of blood-vessel diameter and nerve sensitivity to cold stimuli. Treatment primarily focuses on reducing the frequency of attacks and severity of symptoms. Options may include medications, lifestyle changes, or, in severe cases, surgical intervention.
Symptoms
The symptoms of Raynaud’s phenomenon can vary in severity and duration from person to person, but they generally follow a pattern during an episode.
Common symptoms of Raynaud’s phenomenon include:
- Color Changes: One of the hallmark signs of Raynaud’s phenomenon is the change in the color of the affected extremities, which usually occurs in response to cold temperatures or emotional stress. These color changes can include:
- Pallor (White): The affected fingers or toes often turn white as the blood vessels constrict or narrow, causing a reduction in blood flow.
- Cyanosis (Blue or Purple): As the episode progresses, the lack of oxygen in the blood can cause the affected areas to turn blue or purple.
- Rubor (Red): When blood flow eventually returns to the extremities, they may turn red, sometimes accompanied by a warm sensation.
- Numbness and Tingling: During a Raynaud’s episode, individuals commonly experience numbness and tingling in the affected fingers or toes. This sensation can be uncomfortable and may spread to the hands or feet.
- Pain and Throbbing: Many people with Raynaud’s phenomenon report pain and throbbing in the affected areas. This discomfort can vary in intensity and may persist for the duration of the episode.
- Sensitivity to Cold: Individuals with Raynaud’s phenomenon often have an increased sensitivity to cold temperatures. Exposure to cold air or cold water can trigger an episode.
- Triggers: Raynaud’s episodes can be triggered by various factors, including cold weather, touching cold objects, exposure to freezing water, and emotional stress. Identifying and avoiding these triggers can help manage the condition.
- Duration: Raynaud’s attacks typically last for a short period, ranging from minutes to hours. Once the trigger is removed or the episode subsides naturally, the affected extremities usually return to their normal color and sensation.
It’s important to note that the severity and frequency of Raynaud’s phenomenon can vary from person to person. Some individuals may only experience mild, infrequent episodes, while others may have more frequent and severe attacks. In cases of primary Raynaud’s, the condition is generally less severe and not associated with underlying medical issues, whereas secondary Raynaud’s is often more severe and linked to an underlying medical condition.
Diagnosis
Diagnosing Raynaud’s phenomenon typically involves a combination of medical history assessment, physical examination, and sometimes specialized tests to rule out other conditions and confirm the presence of Raynaud’s.
Diagnostic process for Raynaud’s phenomenon includes:
- Medical History: Your healthcare provider will begin by taking a detailed medical history, including information about your symptoms, their frequency, and any potential triggers or patterns. They will also inquire about your overall health and any underlying medical conditions, as secondary Raynaud’s can be associated with other illnesses.
- Physical Examination: A physical examination is performed to assess the color, temperature, and circulation in your fingers and toes. The doctor will look for characteristic color changes during an episode and may check for any skin ulcers or other signs of tissue damage.
- Differential Diagnosis: Because the symptoms of Raynaud’s phenomenon can overlap with other medical conditions, your healthcare provider will consider alternative diagnoses and may perform tests to rule out other diseases. These conditions can include peripheral artery disease, blood clotting disorders, and autoimmune diseases like systemic sclerosis or lupus.
- Laboratory Tests: Blood tests may be ordered to check for markers of autoimmune diseases or other underlying medical conditions. For example, tests for antinuclear antibodies (ANA) or erythrocyte sedimentation rate (ESR) can provide clues if secondary Raynaud’s is suspected.
- Cold Stress Test: In some cases, a cold stress test may be conducted. During this test, your hands or feet are exposed to cold temperatures, and your healthcare provider monitors your response. This test can help confirm the diagnosis of Raynaud’s if you exhibit the characteristic color changes and symptoms during the exposure.
- Capillaroscopy: This is a non-invasive test that involves examining the small blood vessels (capillaries) in the nailbeds under a microscope. Changes in the capillaries can be indicative of underlying conditions like systemic sclerosis.
- Imaging Studies: In certain situations, imaging studies like Doppler ultrasound or angiography may be recommended to assess blood flow and detect any structural abnormalities in the blood vessels.
It’s important to note that there are two main types of Raynaud’s phenomenon:
- Primary Raynaud’s: This form occurs on its own without an underlying medical condition. It is often milder and typically does not lead to tissue damage.
- Secondary Raynaud’s: This form is associated with an underlying medical condition, such as autoimmune diseases or vascular disorders. It is usually more severe and requires additional investigation to identify and manage the underlying cause.
Once a diagnosis of Raynaud’s phenomenon is confirmed, your healthcare provider will work with you to develop a personalized treatment plan. Treatment may include lifestyle modifications, such as avoiding triggers and keeping extremities warm, and, in some cases, medications to help dilate blood vessels and reduce the frequency and severity of episodes. If an underlying condition is present, treating that condition is also essential to managing Raynaud’s phenomenon effectively.
Treatment Options
The treatment of Raynaud’s Phenomenon depends on its severity and whether it is primary or secondary. For most people, Raynaud’s Phenomenon is not disabling, but it can affect quality of life1. Treatment options include:
Lifestyle and dietary changes:
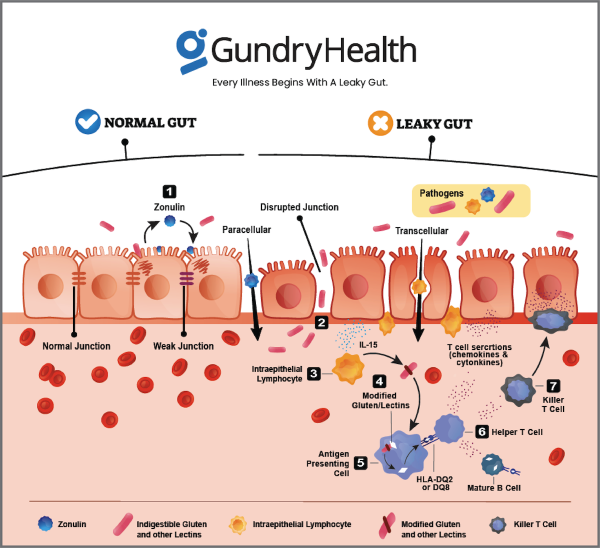
Maintain a Balanced Diet: Avoid Lectin rich foods. Lectins can create a leaky gut by punching holes in your intestinal walls and cause dangerous bacteria and viruses to leak into your bloodstream. The result is widespread inflammation — exactly the kind that can lead to a myriad of autoimmune diseases.
A well-balanced diet that includes a variety of fruits, vegetables, lean proteins, and healthy fats is essential for overall health. A healthy diet can support your cardiovascular system, which is important for managing Raynaud’s.
Stay Hydrated: Proper hydration is essential for maintaining blood flow and overall circulation. Drink plenty of water throughout the day to prevent dehydration, which can exacerbate Raynaud’s symptoms.
Limit Caffeine and Alcohol: Excessive caffeine and alcohol consumption can constrict blood vessels, potentially worsening Raynaud’s symptoms. Consider reducing your intake of coffee, tea, and alcohol, especially during cold weather.
Omega-3 Fatty Acids: Foods rich in omega-3 fatty acids, such as fatty fish (Alaskan salmon, mackerel, sardines), flaxseeds, and walnuts, may have anti-inflammatory properties that can benefit vascular health.
Magnesium: Some individuals find that magnesium-rich foods, like leafy greens, nuts, seeds, and whole grains, may help with circulation and muscle relaxation.
Garlic: Garlic is known for its potential to improve circulation and lower blood pressure. Including garlic in your diet, either in cooking or as a supplement (under medical supervision), may be beneficial.
Ginkgo Biloba: Ginkgo biloba is an herbal supplement that some people with Raynaud’s phenomenon find helpful for improving circulation. However, always consult with a healthcare professional before using supplements, as they can interact with medications or other medical conditions.
Maintain a Healthy Weight: Obesity can worsen circulation problems, so maintaining a healthy weight through a balanced diet and regular exercise is important.
Spicy Foods: Some individuals report that consuming spicy foods, which contain capsaicin, can help improve circulation and reduce the frequency of Raynaud’s episodes. However, this effect can vary from person to person.
Warm Foods and Beverages: During cold weather, consuming warm foods and beverages, such as soups, herbal teas, and hot water with lemon, can help keep your body warm and reduce the risk of triggering an episode.
Medications: Calcium channel blockers, such as nifedipine, are the first choice when medication is needed. Topical nitroglycerin has also been found to help if applied locally4.
- Alternative medicine: Fish oil supplements and ginkgo supplements could help increase blood flow and lessen the number of attacks2.
The Role of Gundry Health
Gundry Health offers a holistic approach to managing Raynaud’s phenomenon. Our services include personalized clinical care, lab results tracking, and a mobile app. Features like food logging, yes-no food lists, and patient care connect patients to specialists.
- Personalized Clinical Care: Our team of specialists provides personalized care plans based on individual health profiles.
- Mobile App: Our mobile app allows patients to track their symptoms, medication, and more, right from their smartphones.
- Food Logging and Yes-No Food Lists: These features help patients identify potential dietary triggers and ensure they’re getting the nutrients they need.
Real-World Success Stories
Many Raynaud’s patients have seen significant improvements in their health outcomes through Gundry Health’s personalized clinical care. For instance, Sarah, a long-term sufferer of Raynaud’s, reported fewer and less severe attacks after using our services for six months. She credits the food logging feature and the personalized care plan for her improved health.
A thorough understanding of the patient experience of Raynaud’s Phenomenon is essential to ensuring that patient-reported outcome (PRO) instruments capture domains important to the target patient population5. Patients with Raynaud’s Phenomenon report numbness of the fingers as the most commonly associated subjective symptom6. A multinational qualitative research study exploring the patient experience of Raynaud’s Phenomenon in systemic sclerosis found that patients experienced a range of symptoms, including pain, numbness, and tingling, and that the condition had a significant impact on their daily lives7.
Proactive Management of Autoimmune Diseases
Managing an autoimmune disease like Raynaud’s requires a proactive approach. At Gundry Health, we believe in empowering patients with tools and resources to manage their health effectively. Whether it’s through personalized care plans, innovative mobile tracking, or dietary guidance, we’re committed to helping you navigate your health journey.
In conclusion, Raynaud’s Phenomenon is a condition that affects the blood vessels in the fingers, toes, ears, and nose, causing them to narrow and reduce blood flow in response to cold temperatures or stress. The exact cause is unknown, but it is believed to be related to the narrowing of blood vessels. Treatment options include lifestyle changes, medications, and alternative medicine. Real-life patient experiences show that Raynaud’s Phenomenon can have a significant impact on daily life. If you experience any of the symptoms of Raynaud’s Phenomenon, it is important to see your doctor for diagnosis and treatment.
Remember, everyone’s experience with Raynaud’s is unique. It’s essential to work closely with your healthcare provider to develop a treatment plan that works best for you. At Gundry Health, we’re here to support you every step of the way.
Get personalized care and recommendations for Raynaud’s Phenomenon from Dr Gundry-Approved program
If you’re looking for more guidance about Raynaud’s Phenomenon than this short list of recommendations, Dr. Gundry’s unique health program is now available to you (without needing an appointment at one of Dr. Gundry’s two, waitlist-only West Coast clinics).
Thanks to the pioneering work of Dr. Gundry and his team at Gundry Health, patient care team trained in Dr. Gundry’s unique holistic methods are now available to help you craft your own personalized Raynaud’s Phenomenon program.
It’s easy to get started.
Simply click the link below to get more information about personalized Raynaud’s Phenomenon treatment plan options, so you can get expert analysis, diagnostic care, and a plan for tackling Raynaud’s Phenomenon, arthritis, or other autoimmune diseases.
Each patient care team member at Gundry Health is Board Certified and trained in Dr. Gundry’s renowned approach to functional medicine and care.
Get your personal lab data and talk to a U.S. licensed doctor. Click Here.