Psoriatic Arthritis: Symptoms, Causes, and the Role of Gundry Health in Management
Psoriatic arthritis is a chronic autoimmune disease that can have a profound impact on a person’s life. At Gundry Health, we’re committed to providing you with comprehensive information about this condition and innovative solutions to help manage it.
Psoriatic arthritis (PsA) is a chronic inflammatory arthritis associated with psoriasis and is found in about 20% of such patients1. PsA can affect any part of the body, including your fingertips and spine, and can range from relatively mild to severe3.
Understanding the Symptoms of Psoriatic Arthritis
Psoriatic arthritis (PsA) can manifest with a variety of symptoms, and these can vary from person to person in terms of severity and the areas of the body affected. PsA primarily involves joint symptoms, but it can also affect other parts of the body.
Common symptoms of psoriatic arthritis include:
- Joint Pain: Persistent joint pain is one of the hallmark symptoms of PsA. This pain is often described as aching, throbbing, or burning and may be worse in the morning or after periods of inactivity.
- Joint Swelling: Inflamed joints can become swollen and tender to the touch. This swelling is usually a result of the immune system’s inflammatory response in the joints.
- Joint Stiffness: People with PsA often experience stiffness, which can make it difficult to move their joints, particularly in the morning or after resting.
- Fatigue: Chronic inflammation and dealing with the symptoms of PsA can lead to fatigue, which can be quite debilitating.
- Enthesitis: Enthesitis is the inflammation of the areas where tendons or ligaments attach to bone. This can lead to pain and tenderness in these areas, such as the heels, the bottoms of the feet, or the elbows.
- Dactylitis: Dactylitis is the swelling of an entire finger or toe, giving it a sausage-like appearance. It’s a characteristic feature of PsA.
- Nail Changes: Psoriatic arthritis can cause changes in the nails, such as pitting (small dents or depressions), ridges, or separation of the nail from the nail bed.
- Skin Symptoms: As PsA is often associated with psoriasis, individuals with PsA may also experience skin symptoms, such as red, scaly, or silvery patches of skin. These skin symptoms can occur independently of joint symptoms.
- Eye Inflammation: In some cases, PsA can cause inflammation in the eyes, leading to redness, pain, and blurred vision.
- Back Pain: Psoriatic spondylitis is a form of PsA that affects the spine. It can cause lower back pain and stiffness, and in severe cases, it may lead to spinal fusion.
- Reduced Range of Motion: Over time, PsA can lead to joint damage and deformities, which can result in a reduced range of motion and difficulty performing everyday tasks.
It’s important to note that PsA can vary widely in its presentation. Some individuals may experience mild, intermittent symptoms, while others may have more severe and persistent joint involvement.
The Importance of Early Diagnosis
Early diagnosis and ongoing monitoring are crucial for managing psoriatic arthritis. Without treatment, this condition can lead to permanent joint damage. Regular check-ups can ensure that your treatment plan is working and can be adjusted as needed.
No single test can confirm a diagnosis of PsA, but some types of tests can rule out other causes of joint pain, such as rheumatoid arthritis or gout6. During the exam, your doctor might examine your joints for signs of swelling or tenderness, check your fingernails for pitting, flaking, and other abnormalities, and press on the soles of your feet and around your heels to check for tender areas6. Imaging tests such as X-rays and MRI can help pinpoint changes in the joints that occur in PsA but not in other arthritic conditions6.
How Gundry Health Can Help
At Gundry Health, we’re proud to offer a unique tool designed to aid in the diagnosis and management of psoriatic arthritis. Its features include:
- Mobile App: Keep track of your symptoms, medication, and more, right from your smartphone.
- Personalized Clinical Care: Receive personalized care plans based on your unique health profile and needs.
- Food Logging: Monitor your diet to identify potential triggers and ensure you’re getting the nutrients you need.
Dr. Gundry’s Treatment Approach
Dr. Gundry embarked on a quest to unravel the root causes of autoimmune diseases, particularly seeking to aid patients grappling with psoriatic arthritis. His journey unveiled a common thread shared by all his patients—a thread that can be traced back to a seemingly innocuous over-the-counter painkiller.
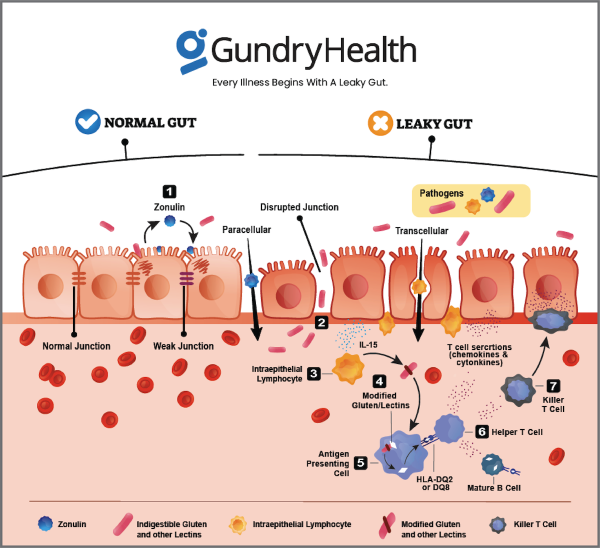
Indeed, numerous non-prescription painkillers have a rather insidious side effect: they compromise the integrity of the gut lining. Dr. Gundry paints a vivid analogy, likening non-steroidal anti-inflammatory drugs (NSAIDs) to virtual “hand grenades” detonating breaches within your gut.
Dr. Gundry further discerned a singular culprit lurking within the diets of many of his patients—a protein known as lectin. These ubiquitous proteins, abundant in everyday foods like tomatoes, potatoes, and certain whole grains, were suspected to be the chief architects behind the frailty of the gut lining.
Lectins, as it turns out, are the natural defenses of plants against potential predators. Unfortunately, the human gastrointestinal tract struggles to fully break them down. This struggle culminates in disrupted digestion, impaired nutrient absorption, immune system inflammation, and a perturbed microbiome balance, where the harmonious community of gut bacteria faces disruption.
To compound matters, lectins possess the unnerving ability to perforate intestinal walls, resulting in their unwelcome entry into the bloodstream. This phenomenon triggers a cascade of widespread inflammation—a potent catalyst for the onset of autoimmune disorders, including the likes of psoriatic arthritis.
Ways to Alleviate Psoriatic Arthritis Discomfort
If you’ve received a diagnosis of psoriatic arthritis or suspect you may be dealing with it, you can follow a series of straightforward steps to bid farewell to your pain once and for all.
- Ditch Processed Fare: Steer clear of packaged and processed foods; they constitute a significant portion of many Americans’ diets and are brimming with sugar, artificial additives, and other inflammatory substances. The more you indulge in them, the greater your vulnerability to autoimmune diseases, exacerbating your condition further.
- Embrace Wholesome Nourishment: Prioritize whole foods, especially high-fiber vegetables such as onions, asparagus, and artichokes. These natural, unprocessed foods supply your gut with nourishing starches and fiber that promote fullness and enhance the well-being of your microbiome—the beneficial microorganisms inhabiting your gut.
- Opt for Natural Sweetness: Sugar ranks among the most detrimental items in your diet, serving as a catalyst for inflammation and obesity, and it lurks in almost all packaged and processed foods. However, for those with a sweet tooth, Dr. Gundry suggests savoring low-fructose seasonal fruits in moderation. His preferred choices include wild berries, skin-on kiwifruit, pomegranates, passion fruit, and grapefruit.
- Banish Lectins: These bothersome plant proteins can precipitate a leaky gut. Notable sources of lectins include specific nightshade vegetables (like tomatoes, potatoes, and eggplants), certain nuts and seeds such as cashews and peanuts, and legumes and beans. Dr. Gundry’s lectin remedy: you can completely neutralize lectins in most of these foods by employing a pressure cooker.
- Don’t Overlook Fiber: For fostering a healthier gut, prioritize prebiotic fiber—an excellent choice for your digestive well-being. Among the top prebiotics is inulin, readily found in foods like chicory, asparagus, onions, leeks, and artichokes. Dr. Gundry’s “refrigerator trick” for obtaining more prebiotic fiber from starchy foods like yams, sorghum, millet, and pressure-cooked rice entails cooking, chilling, and reheating them before consumption.
By following these uncomplicated steps, you can embark on a journey toward alleviating the discomfort associated with psoriatic arthritis and improving your overall well-being.
Living with psoriatic arthritis requires a proactive approach. Here are some practical tips:
- Stay Active: Regular exercise can help keep your joints flexible.
- Eat Healthily: A balanced diet can help manage inflammation and support overall health.
- Manage Stress: Mind-body techniques such as yoga and meditation can help reduce stress, which can exacerbate symptoms.
Remember, everyone’s experience with psoriatic arthritis is unique. It’s important to work closely with your healthcare provider to develop a treatment plan that works best for you. At Gundry Health, we’re committed to supporting you every step of the way on your journey towards better health.
Get personalized care and recommendations for Psoriatic Arthritis from Dr Gundry-Approved program
If you’re looking for more guidance about Psoriatic Arthritis disease than this short list of recommendations, Dr. Gundry’s unique health program is now available to you (without needing an appointment at one of Dr. Gundry’s two, waitlist-only West Coast clinics).
Thanks to the pioneering work of Dr. Gundry and his team at Gundry Health, patient care team trained in Dr. Gundry’s unique holistic methods are now available to help you craft your own personalized Psoriatic Arthritis program.
It’s easy to get started.
Simply click the link below to get more information about personalized Psoriatic Arthritis treatment plan options, so you can get expert analysis, diagnostic care, and a plan for tackling Psoriatic Arthritis, arthritis, or other autoimmune diseases.
Each patient care team member at Gundry Health is Board Certified and trained in Dr. Gundry’s renowned approach to functional medicine and care.
Get your personal lab data and talk to a U.S. licensed doctor. Click Here.