A New Approach for Psoriasis Treatment: Dr. Steven Gundry Explains Surprising Cause of this Autoimmune Disease
Discover more about the signs and symptoms of psoriasis, the different types of psoriasis, and a novel new method for treating this autoimmune disease.
What is psoriasis? Is Psoriasis an autoimmune disease?
Psoriasis is a chronic autoimmune disease that causes your skin cells to rapidly build up. This typically leads to a rash with itchy, scaly patches on your skin’s surface. Inflammation and redness around these scaly patches are common. Scaly patches most often appear on the scalp, face, hands, feet, and neck.
In the United States, psoriasis affects around 7.5 million adults (a 3% prevalence rate).1 And psoriasis is commonly associated with a number of other conditions, including type 2 diabetes, heart disease, inflammatory bowel disease, psoriatic arthritis, and anxiety/depression.
What are the signs and symptoms of psoriasis?
While the severity of psoriasis symptoms can vary from person to person, common signs include some of the following:
- A patchy rash or rashes that can lead to small scaling or major eruptions all over your body
- Raised, inflamed patches (these will typically appear red on white skin or purple/brown on darker skin)
- Dry, cracked skin (that can often lead to bleeding)
- Itching and burning around the patches
- Rashes that appear for a few weeks or months, disappear, and then reappear again
- Painful, swollen joints
What are the different types of psoriasis?
There are actually several different types of psoriasis, and each one has its own unique signs and symptoms. These include:
Plaque psoriasis – This is the most common type of psoriasis. It’s estimated around 80-90 percent of people with psoriasis have plaque psoriasis. Plaque psoriasis causes dry, itchy, raised skin patches (plaques) covered with scales.
Guttate psoriasis – This type of psoriasis commonly affects children and young adults. Guttate psoriasis causes small, tear-drop shaped pink or violet spots to appear on the skin. It commonly appears after a bacterial infection like strep throat.
Pustular psoriasis – Rarer and more common in adults, pustular psoriasis causes white, pus-filled blisters to appear in patches on the palms or soles.
Inverse psoriasis – This form of psoriasis mainly affects the skin folds of the groin, buttocks, and breast. It’s characterized by bright areas of red, shiny, inflamed skin (or a more intense purple/violet color on darker skin tones). Symptoms can worsen with friction and sweating.
Erythrodermic psoriasis – This very rare form of psoriasis can cause an itchy, burning, peeling rash to cover the entire body (making the skin appear sunburned). This form is serious enough it can cause illness or fever, so if you’re experiencing any of these symptoms be sure to consult a doctor immediately.
What is the difference between psoriasis and eczema?
While eczema may or may not be a form of autoimmune disease, psoriasis is widely considered an autoimmune disease. This means that part of the body’s own immune system becomes overactive and starts attacking the body’s tissues. Other examples of autoimmune diseases include arthritis, Hashimoto’s thyroiditis, and lupus (among others).
While both eczema and psoriasis symptoms can appear rashy or scaly, psoriasis patches tend to be thicker and more inflamed. That’s because psoriasis is caused by a rapid buildup of cells on the surface of the skin.
If you’re still unsure if you’re suffering from eczema or from psoriasis, be sure to consult a dermatologist for a more accurate diagnosis.
What causes psoriasis?
Psoriasis is a type of autoimmune condition, which means it’s caused by an overactive immune system that begins attacking the body’s own tissues. Like many other autoimmune diseases, including arthritis, it’s often unclear what initially leads to the autoimmune disease.
Recent research also indicates that there may be a genetic factor to whether someone gets psoriasis. According to one 2019 paper, if you have an immediate family member with psoriasis, you have an increased risk of getting the disease.2
However, there is some evidence that autoimmune diseases are actually caused by treatable environmental factors. This theory, championed by cardiothoracic surgeon Dr. Steven Gundry and others, could help millions of people get rid of their psoriasis for good (more on this below).
Understanding the gut-skin axis
There may be a surprising “silver bullet” for treating psoriasis, although it’s something scientists are still investigating. It’s called the gut-skin axis, and it refers to the surprising relationship between your gut – including your digestive system and all the bacteria and microorganisms that call your gut home, collectively called your microbiome – and your skin.
Put simply, your gut actually is in constant communication with other parts of your body, including your skin. So when any aspect of your delicate microbiome is out-of-balance, the health of your entire body can suffer – including the health of your skin.
In fact, scientists have found that people with some skin conditions have different bacteria in their gut and different bacteria on their skin than people without these conditions. But how and why does this happen?
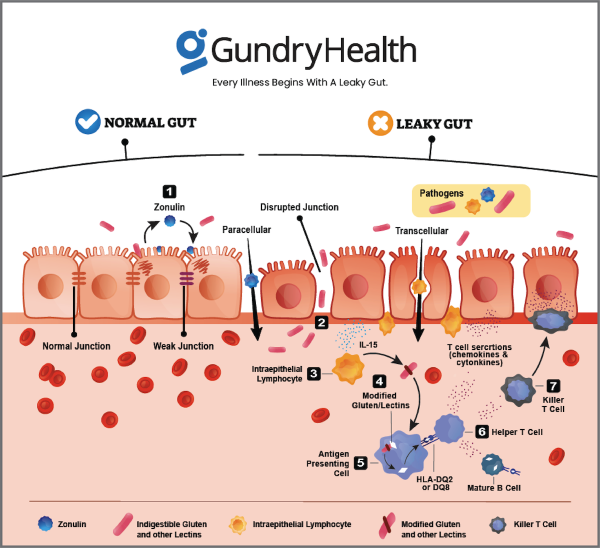
You see, the immune cells along your gut lining play an important role in keeping your gut wall strong. They decide what can leave the GI tract and what must stay contained.
When everything is working well, nothing gets through this strong gut barrier except what’s supposed to. However, when this barrier gets worn down (more on that below) and develops more and more microscopic holes, it allows other compounds to “leak” through, causing your health to suffer.
Is psoriasis a symptom of leaky gut?
This is the condition known as “leaky gut.”
So when the wrong molecules or even bacteria get across the border of your gut wall, your immune system kicks into high gear. Normally, this is really important since your immune system can call in “reinforcements” – inflammatory hormones called cytokines. These cytokines can save your life from a bacterial infection and help you heal when you have an injury.
The problem starts when your immune system starts responding to every little thing. Think of it like an overactive security alarm system. You’re grateful when it alerts you to the presence of a thief, but you’re annoyed when it goes off every time a fly enters your home.
That’s exactly what happens when you have a leaky gut. Your immune system begins responding to everything that gets through your porous gut wall. This leads to chronic inflammation – including the kind of inflammation on your skin that causes psoriasis.
In other words, a leaky gut – which is often caused by environmental triggers like certain foods, chemicals, or stress – leads directly to psoriasis.
How to treat psoriasis – a new approach
In order to start reducing your psoriasis symptoms, you need to understand what causes a leaky gut in the first place. When you take care of the problem at the source, you can dramatically lessen the frequency and severity of your psoriasis.
Imagine your body is a fortress. You need a wall to protect yourself. That’s your gut wall. Immune cells are the soldiers there to protect your fortress. Their job is to detect friend from foe. And when they fight for you, they cause collateral damage. We call that collateral damage inflammation.
However, your protective walls aren’t sealed shut. All along the wall are tiny doors. And while these doors are closed most of the time, sometimes they need to open to allow food or friends to come in.
So imagine what would happen if those doors were always open. It would be much harder for your soldiers to defend the fortress (your body). Now, there is a molecule (called zonulin) inside your body that makes these “doors” in your gut wall open or close. And there are certain environmental triggers that make your cells produce zonulin.
One such trigger is a type of protein called a lectin. Plants produce lectins as a defense against being eaten. In fact, lectins are so powerful they can even paralyze the bugs that eat them.
Of course, you’re a lot bigger and stronger than a little bug. And you have your own defense mechanisms, like mucus, which can bind to lectin proteins and make them harmless as you digest them.
However, as humans have consumed more and more lectin-rich foods (like tomatoes, potatoes, beans, and most grains) our natural defenses against these pesky proteins have begun to weaken.
And when lectins make it through to your GI tract, they can cause all kinds of problems. For one, they bind with receptors along the gut lining to produce zonulin. As explained above, zonulin then breaks the tight junctions holding together your gut wall. This creates spaces between the cells for “foreign invaders” (like harmful bacteria) to get through and get to other parts of your body.
The result? Inflammation.
This is why reducing lectin consumption is a major part of Dr. Gundry’s health program. (Click HERE to find a complete list of lectin-containing foods you should avoid if you’re suffering from psoriasis.)
Dr. Gundry has helped tens of thousands of his patients from around the world – and many more people via his best-selling books like Longevity Paradox – to get rid of their autoimmune diseases, including psoriasis. He’s done this by utilizing the latest blood and laboratory tests and combining these test results with a comprehensive personalized diet and nutrition program.
Get personalized care and recommendations for eczema from Dr. Gundry-Approved care coordinators
If you’re looking for more guidance about psoriasis, Dr. Gundry’s unique health program is now available to you (without needing an appointment at one of Dr. Gundry’s two waitlist-only West Coast clinics).
Thanks to the pioneering work of Dr. Gundry and his team at Gundry Health, care coordinators trained in Dr. Gundry’s unique holistic methods are now available to help you craft your own personalized psoriasis program.
——-
1 Armstrong AW, Mehta MD, Schupp CW, Gondo GC, Bell SJ, Griffiths CEM. Psoriasis Prevalence in Adults in the United States. JAMA Dermatol. 2021;157(8):940-946. doi:10.1001/jamadermatol.2021.2007
2 Huang YH, Kuo CF, Huang LH, Hsieh MY. Familial Aggregation of Psoriasis and Co-Aggregation of Autoimmune Diseases in Affected Families. J Clin Med. 2019;8(1):115. Published 2019 Jan 18. doi:10.3390/jcm8010115