Polycystic Ovary Syndrome – PCOS: A Comprehensive Overview by Gundry Health
Polycystic Ovarian Syndrome (PCOS) stands as the most prevalent endocrine disorder affecting females. It significantly contributes to menstrual irregularities and reproductive age infertility. The development of PCOS is deeply influenced by genetic and hormonal factors. In this disorder, a reduced level of progesterone prompts an excessive immune response, resulting in heightened estrogen production, which, in turn, triggers the production of various autoantibodies.
PCOS has been associated with the emergence of different autoantibodies, including but not limited to anti-nuclear (ANA), anti-thyroid, anti-spermatic, anti-SM, anti-histone, anti-carbonic anhydrase, anti-ovarian, and anti-islet cell antibodies. Notably, there is a recognized link between PCOS and autoimmune diseases such as ANA and anti-TPO, which have also been observed in systemic lupus erythematosus and Hashimoto’s thyroiditis, respectively. These findings raise suspicions that certain autoantibodies may exert an influence on the long-term clinical management of individuals with PCOS.
The presence of fluctuating levels of autoantibodies among different PCOS patients opens the door to new avenues of research at the molecular level. This promising exploration may ultimately lead to the discovery of improved treatment options for PCOS in the near future.
Defining PCOS & Its Symptoms
Polycystic Ovary Syndrome (PCOS), will typically manifest in patient late teens or early twenties. It’s important to note that not all individuals with PCOS will display every symptom, and the severity of each symptom can vary widely.
Common symptoms of PCOS include:
- Irregular Menstrual Cycles: Many individuals with PCOS have irregular periods or may not have them at all.
- Fertility Challenges: PCOS is a leading cause of female infertility. It often results in irregular or absent ovulation, making it difficult for affected individuals to conceive.
- Excessive Hair Growth (Hirsutism): Hair may grow excessively in male-pattern areas such as the face, chest, back, or buttocks.
- Weight Gain: Weight gain is a common issue among those with PCOS.
- Hair Thinning and Loss: Individuals with PCOS may experience hair thinning and loss, particularly from the scalp.
- Oily Skin and Acne: Skin issues like oily skin and acne are often associated with PCOS.
If you identify with any of these symptoms and suspect you may have PCOS, it is advisable to consult with your general practitioner (GP) for further evaluation and guidance.
Fertility Concerns
PCOS is a prevalent cause of female infertility, and many women discover they have PCOS when they encounter difficulties conceiving. In a typical menstrual cycle, the ovaries release an egg into the uterus through ovulation, which usually occurs once a month. However, individuals with PCOS may experience
Causes
PCOS is caused by an imbalance of reproductive hormones. The hormonal imbalance creates problems in the ovaries, which make the egg that is released each month as part of a healthy menstrual cycle. With PCOS, the egg may not develop as it should or it may not be released during ovulation as it should be. PCOS can cause missed or irregular menstrual periods. Irregular periods can lead to infertility.
The exact cause of PCOS is unknown, but it’s considered that several factors, including genetics, play a role:
- Insulin resistance: Over 50% of women with PCOS have insulin resistance, contributing to increased androgen production by the ovaries.
- Inflammation: Women with PCOS often have increased levels of inflammation, which has been linked to higher androgen levels.
- Heredity: Research suggests that PCOS can run in families.
Diagnostic Tests for PCOS
Diagnosing Polycystic Ovary Syndrome (PCOS) typically involves a combination of clinical evaluation, medical history, physical examinations, and specific tests. The process can vary slightly among healthcare providers, but here is a general overview of how PCOS is diagnosed:
Medical History and Symptom Assessment:
Your healthcare provider will start by discussing your medical history, including your menstrual cycles, symptoms you’ve been experiencing, and any relevant family history.
They will inquire about the frequency and regularity of your periods, as well as any issues related to fertility, acne, excessive hair growth, and weight changes.
Physical Examination:
A physical examination may be performed to assess for signs of PCOS, such as excessive hair growth (hirsutism), acne, and abdominal obesity.
Blood Tests:
Blood tests may be conducted to measure hormone levels. Common hormone tests include:
Follicle-Stimulating Hormone (FSH): This hormone helps regulate the menstrual cycle.
Luteinizing Hormone (LH): Elevated LH levels in relation to FSH levels are a common characteristic of PCOS.
Testosterone: High levels of this male hormone can lead to hirsutism and other PCOS symptoms.
Insulin: Insulin resistance is often associated with PCOS and can be assessed through fasting insulin levels and glucose levels.
Imaging Studies:
Transvaginal Ultrasound: A pelvic ultrasound may be performed to examine the ovaries. In PCOS, the ovaries often appear enlarged and contain multiple small cysts or follicles, which may be visible on the ultrasound.
Rule Out Other Conditions:
Your healthcare provider may perform tests to rule out other conditions that can mimic PCOS symptoms, such as thyroid disorders or adrenal gland disorders.
Rotterdam Criteria:
The Rotterdam criteria are often used for diagnosing PCOS. According to these criteria, a diagnosis of PCOS is made if at least two of the following three criteria are met:
Irregular or absent menstrual cycles.
Clinical or laboratory evidence of hyperandrogenism (excess male hormones) such as hirsutism or elevated testosterone levels.
Polycystic ovaries on ultrasound (12 or more follicles in each ovary measuring 2-9 mm in diameter or an increased ovarian volume).
It’s important to note that there is no single test that definitively diagnoses PCOS. Instead, it is a combination of clinical evaluation, medical history, hormone levels, and ultrasound findings. Additionally, the diagnosis should be made by a healthcare professional with expertise in PCOS, such as a gynecologist or endocrinologist.
Once diagnosed, the treatment approach will depend on the individual’s specific symptoms and goals, which may include managing menstrual irregularities, addressing fertility concerns, and addressing other PCOS-related health issues like insulin resistance and acne.
Preventing PCOS through Lifestyle Changes
While you can’t prevent PCOS, you can certainly lower your risk and manage the impact of symptoms through lifestyle changes. Regular exercise, a healthy diet, weight control, and not smoking are all important parts of treatment for PCOS.
Treating PCOS & Gundry Health Approach
Treatment for PCOS may include lifestyle modifications, medication, and in some cases, surgery.
- Weight Loss: Maintaining a healthy weight is crucial for controlling PCOS symptoms. Many individuals with PCOS carry extra weight, which can elevate the risk of diabetes, heart disease, and metabolic syndrome. Losing just 5% of body weight can alleviate PCOS symptoms. Lifestyle changes like a balanced diet and increased physical activity can aid in weight loss and reduce health-related risks.
- Dietary Adjustments: Altering one’s diet is integral to PCOS management. People with PCOS often have elevated insulin levels, a hormone that regulates blood sugar. Consistently high insulin levels can lead to insulin resistance, a precursor to diabetes.
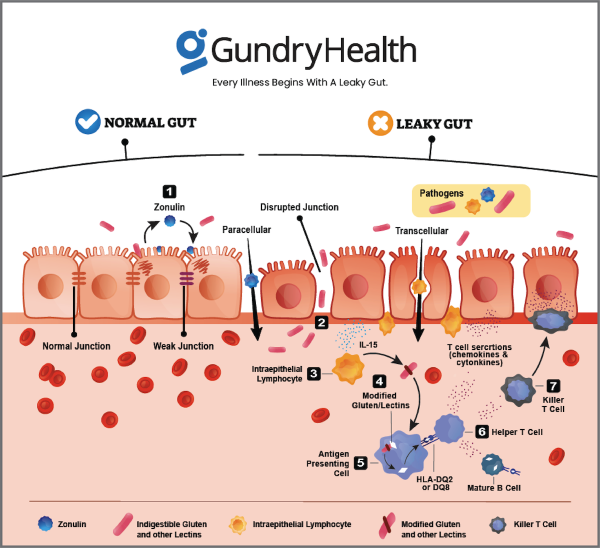
Adopt a well-rounded diet that prioritizes plant-based foods, healthy fats, and lean proteins. Steer clear of items abundant in sugar, refined carbohydrates, lectins, gluten, dairy, soy, corn, and nightshades, as these can potentially instigate conditions like leaky gut syndrome, inflammation, disturbances in your gut microbiome, and compromise your immune system. Recent research suggests that the ketogenic or “keto” diet may alleviate symptoms. This dietary regimen entails minimizing carbohydrate intake and deriving energy primarily from fats.
- Exercise: Regular physical activity is a key component of weight loss and PCOS management. Exercise helps lower insulin levels and maintains stable blood sugar levels. It also promotes heart health, enhances mood, and regulates sleep patterns. The most effective exercise regimen is one that is enjoyable and sustainable.
- Supplements: Some individuals turn to nutritional supplements to address PCOS symptoms. It’s important to note that these supplements are not FDA-regulated and may interact with medications or medical conditions. While research regarding their effectiveness and safety varies, there is limited evidence suggesting benefits from supplements like omega-3 fish oil and inositol for some PCOS patients.
- Herbal Products: Certain herbal supplements are popular among PCOS patients. Studies have indicated that Vitex agnus-castus and Cimicifuga racemosa may assist in managing irregular ovulation and related infertility. Cinnamomum cassia may also be beneficial for treating metabolic complications associated with PCOS. Herbal products are not FDA-regulated and should be used cautiously.
- CBD: Cannabidiol (CBD) oil, derived from the Cannabis sativa plant, has garnered interest for various health conditions, including PCOS. While research on CBD and PCOS is in its early stages, it has shown potential for addressing anxiety and insomnia, common issues in PCOS patients.
- Probiotics: Recent research has linked gut microbiome alterations to various diseases, including PCOS. Probiotic supplements were found to reverse PCOS symptoms in animal studies. While further research is needed, probiotics are generally considered safe and may have potential benefits in PCOS management.
Medical
- Medications: Birth control pills can help regulate menstrual cycles and reduce androgen levels. Other medications, such as metformin, clomiphene, and letrozole, may also be prescribed to help regulate ovulation and improve fertility.
- Surgery: In rare cases, surgery may be recommended to remove cysts from the ovaries.
Gundry Health clinical program designed with an innovative approach that may help manage the hormonal imbalance seen in PCOS. Numerous scientific studies suggest that certain foods can balance insulin levels, a key factor in PCOS. However, it’s important to remember that diet should be used as part of a broader treatment plan under professional supervision.
Get personalized care and recommendations for PCOS from Dr Gundry-Approved program
If you’re looking for more guidance about PCOS disease than this short list of recommendations, Dr. Gundry’s unique health program is now available to you (without needing an appointment at one of Dr. Gundry’s two, waitlist-only West Coast clinics).
Thanks to the pioneering work of Dr. Gundry and his team at Gundry Health, patient care team trained in Dr. Gundry’s unique holistic methods are now available to help you craft your own personalized PCOS program.
It’s easy to get started.
Simply click the link below to get more information about personalized PCOS treatment plan options, so you can get expert analysis, diagnostic care, and a plan for tackling PCOS, arthritis, or other autoimmune diseases.
Each patient care team member at Gundry Health is Board Certified and trained in Dr. Gundry’s renowned approach to functional medicine and care.
Get your personal lab data and talk to a U.S. licensed doctor. Click Here.
References