Irritable Bowel Disease (IBD): Dr. Gundry Reveals How to Manage and Treat IBD Naturally
How the autoimmune disease irritable bowel disease is diagnosed (including signs and symptoms), where irritable bowel disease comes from, why irritable bowel disease can get worse, and a landmark new method for treating it without pharmaceuticals
What is irritable bowel disease? Is IBS an autoimmune disease?
Irritable bowel disease refers to a group of autoimmune disorders. These disorders (like Crohn’s disease and ulcerative colitis), cause long-term inflammation of your digestive tract.
Your digestive system breaks down your food, processes nutrients, and removes unwanted waste products. This digestive process is incredibly important to your overall health.
So any inflammation in your digestive tract can lead to a bunch of complications.
Now, as mentioned above, the two most common forms of irritable bowel disease include Crohn’s disease and ulcerative colitis (UC).
Crohn’s disease leads to inflammation of the digestive tract, particularly in the small intestine. Ulcerative colitis also leads to digestive tract inflammation. But UC normally means inflammation only in the lining of the large intestine or rectum. Around 4 million American adults are currently suffering from either Crohn’s disease or ulcerative colitis.
Do I have IBD or irritable bowel disease? Check for these IBD symptoms
Symptoms of irritable bowel disease can vary in frequency and severity.
However, common IBD symptoms may include the following:
- Diarrhea
- Bleeding ulcers (which can lead to blood in your stool)
- Bowel obstruction (leading to problems like frequent stomach pain, cramping, and bloating)
- Weight loss and anemia caused by an inability to absorb nutrients from your food
Irritable bowel disease is even linked to problems occurring outside of the digestive system, including skin disorders (like eczema), arthritis, and eye inflammation.
Causes of Crohn’s and Ulcerative Colitis (why the food you eat can cause IBD)
While the exact cause of most irritable bowel diseases is unknown, there’s now strong evidence that environmental factors play a big role.
According to former cardiothoracic surgeon and New York Times best-selling author Dr. Steven Gundry, there’s one reason so many of his patients come to him with irritable bowel diseases like Crohn’s and UC.
And unsurprisingly, it starts in your gut.
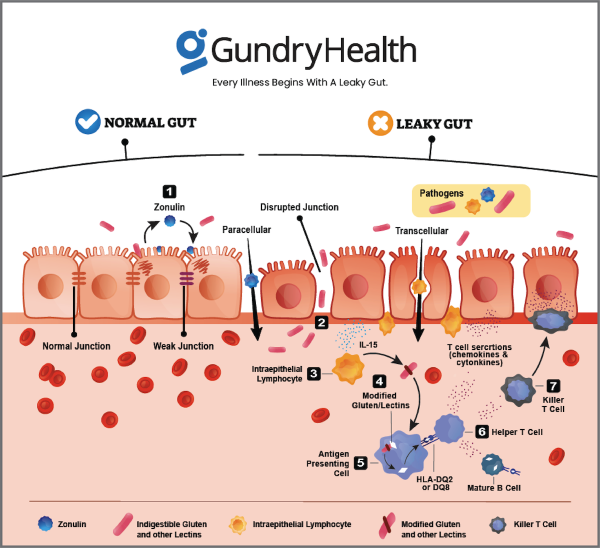
You see, the immune cells along your gut lining play an important role in keeping your gut wall strong. They decide what can leave the GI tract and what must stay contained.
When everything is working well, nothing gets through this strong gut barrier except what’s supposed to. However, when this barrier gets worn down (more on that below) and develops more and more microscopic holes, it allows other compounds to “leak” through, causing your health to suffer.
This is the condition known as “leaky gut.”
Here’s another way to think about it…
Imagine your body is a fortress. You need a wall to protect yourself. That’s your gut wall. Immune cells are the soldiers there to protect your fortress. Their job is to detect friend from foe. And when they fight for you, they cause collateral damage. We call that collateral damage inflammation.
However, your protective walls aren’t sealed shut. All along the wall are tiny doors. And while these doors are closed most of the time, sometimes they need to open to allow food or friends to come in.
So imagine what would happen if those doors were always open. It would be much harder for your soldiers to defend the fortress (your body). Now, there is a molecule (called zonulin) inside your body that makes these “doors” in your gut wall open or close. And there are certain environmental triggers that make your cells produce zonulin.
One of these “triggers” is gluten . Humans, it turns out, were never meant to eat this food. And for most of human history, we didn’t. But once humans stopped living a hunter-gatherer lifestyle and started farming, gluten became a staple of our diets. Which might not have been a problem, except for one thing.
You see, gluten has certain protein “fragments” that humans can’t digest. Because of that, these “fragments” communicate with the soldiers on your gut wall and say, “Please, release zonulin and let us in.” Your immune system, though, thinks these proteins are invaders and starts fighting back. This causes inflammation.
How a leaky gut leads to irritable bowel disease
When the wrong molecules or even bacteria get across the border of your gut wall, your immune system kicks into high gear. Normally, this is really important since your immune system can call in “reinforcements” – inflammatory hormones called cytokines.
These cytokines can save your life from a bacterial infection and help you heal when you have an injury.
The problem starts when your immune system starts responding to every little thing. Think of it like an overactive security alarm system. You’re grateful when it alerts you to the presence of a thief, but you’re annoyed when it goes off every time a fly enters your home.
That’s exactly what happens when you have a leaky gut. Your immune system begins responding to everything that gets through your porous gut wall. This leads to chronic inflammation.
Now here’s what all this has to do with autoimmune diseases like irritable bowel disease. The zonulin gene sits on a certain chromosome linked to many autoimmune diseases, certain types of cancer, and diseases of the nervous system like multiple sclerosis.
So while genetics and your environment do play a role in whether you develop autoimmune diseases like irritable bowel disease, a leaky gut is the crucial third ingredient. This is why it’s so important to keep your gut wall strong. And unlike your genetics, and often unlike your environment, you can fix a leaky gut.
What happens when you DON’T deal with your irritable bowel disease symptoms
If you don’t address your symptoms of irritable bowel disease at the source, it can lead to many long-term complications.
These include malnutrition and weight loss, intestinal rupture (which is as uncomfortable as it sounds), bowel obstruction, and colorectal cancer.
That’s why it’s absolutely critical to notice your symptoms of irritable bowel disease and speak with a doctor or specialist about what you can do to address the problem.
How to treat IBD (according to Dr. Gundry)
If you do suspect you may have irritable bowel disease, or if you’re already suffering from IBD symptoms, there are some steps you can take right at home.
Dr. Gundry always begins with blood work. He looks for specific markers of autoimmune disease (for example, irritable bowel disease) and other key indicators of a bigger problem (like markers for gluten sensitivity).
Next, Dr. Gundry has his irritable bowel disease patients begin his specific dietary program. While this includes cutting gluten from the diet, it also includes cutting other inflammatory foods like sugar and lectins . See Dr. Gundry’s YES / NO Food list for IBD . However, this is not an elimination diet, nor is it about depriving yourself or feeling hungry.
Patients who start this program are often amazed by the result. Like 20 year-old Jill W., one of Dr. Gundry’s former patients:
“After two weeks [on Dr. Gundry’s dietary program], I had the first normal bowel movement of my life, and they have been normal ever since.”