A Cure for Celiac Disease? New York Times Best-Selling Author Dr. Steven Gundry How It’s Possible
Discover why gluten can cause so many health problems, the difference between Celiac Disease and gluten intolerance, and how to deal with symptoms of Celiac Disease.
What is celiac disease?
Celiac disease – sometimes called celiac sprue – is an autoimmune disease that can lead to damage of the small intestine. When people with celiac disease eat gluten – the protein found in foods made of wheat, rye, and barley – their body’s immune system starts attacking the tiny bumps (called villi) that line the small intestine.
The villi in your small intestine help you take nutrients from your food into your bloodstream. Without them, your body can’t get enough nutrients from the food you eat (no matter how much food you consume).
It’s estimated that around one in 100 people worldwide suffer from celiac disease. In the United States, one in 133 people—around 2 million people overall—have celiac disease.
What are the symptoms of celiac disease?
Celiac disease affects everyone differently (some people may experience few or no symptoms well into adulthood). However, common symptoms of celiac disease include:
- Digestive problems – these include abdominal pain, gas, bloating, constipation, diarrhea, and pale stools)
- Weight loss – due to lack of proper nutrient absorption
- Anemia – unexplained low blood count that makes you feel tired all the time
- A tingling sensation in the legs – this is often caused by nerve damage
- Dermatitis herpetiformis – this is a type of painful, itchy skin rash
- Muscle cramps or bone pain
- Teeth changing color or losing their dental enamel
- Infertility
- Depression
If you experience any of these symptoms regularly, be sure to consult your doctor for a biopsy or blood work to determine if you have celiac disease.
What’s the difference between celiac disease and gluten intolerance?
You may have heard of gluten sensitivity before (sometimes called non-celiac gluten sensitivity or NCGS). Gluten sensitivity is a reaction to the protein gluten that leads to gastrointestinal issues, headaches, and brain fog.
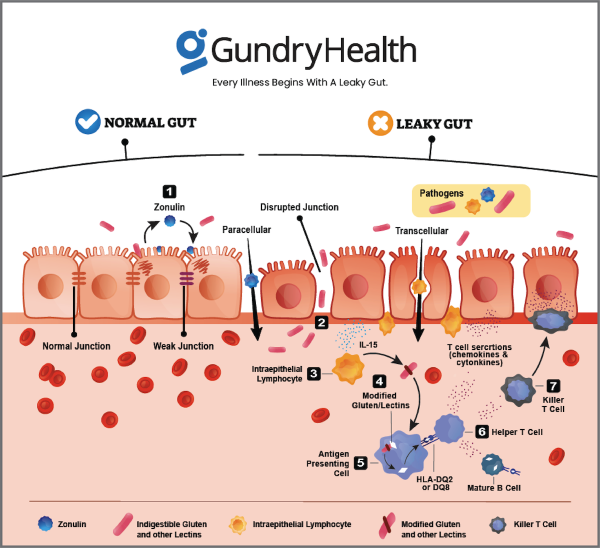
However, unlike celiac disease, gluten sensitivity does not lead to damage of the villi in the small intestine. It may lead to the condition known as leaky gut. Certain proteins – like gluten – can actually force apart the “tight junctions” that make up the lining of your gut wall. Over time, gluten can cause microscopic holes to form in your gut wall, allowing other compounds to “leak” through.
This is the definition of “leaky gut syndrome,” also known as intestinal permeability. And if left untreated, leaky gut can eventually lead to the development of autoimmune diseases like Crohn’s disease, ulcerative colitis, hypothyroidism, lupus, multiple sclerosis, rheumatoid arthritis, psoriasis, and more.
While all of this is certainly bad, there’s not much evidence that gluten sensitivity leads to damage of the small intestine.
What causes celiac disease?
Celiac disease is hereditary. This means it is most often passed down from parent to child. It’s estimated that people with a first-degree relative with celiac disease have a 1 in 10 risk of developing the disease.
In other words, the research suggests celiac disease only affects people with certain genes who consume gluten. And even among people with the genetic markers for celiac disease, only a small percentage actually develop the disease.
What happens when someone with celiac disease eats gluten?
Celiac disease is an autoimmune disease. That means it causes a person’s immune system to mistakenly attack its own body.
So when someone with celiac disease eats gluten, their immune system identifies the protein as a toxic invader and begins attacking the tissue around the small intestine. Over time, this wears down the helpful villi of the small intestine.
When the villi are damaged, the body can no longer properly absorb nutrients. This is why celiac disease can often lead to rapid weight loss, anemia, and stunted growth in children.
Why is gluten so harmful to some people?
Imagine your body is a fortress. You need a wall to protect yourself. That’s your gut wall. Immune cells are the soldiers there to protect your fortress. Their job is to detect friend from foe. And when they fight for you, they cause collateral damage. We call that collateral damage inflammation.
However, your protective walls aren’t sealed shut. All along the wall are tiny doors. And while these doors are closed most of the time, sometimes they need to open to allow food or friends to come in.
So imagine what would happen if those doors were always open. It would be much harder for your soldiers to defend the fortress (your body). Now, there is a molecule (called zonulin) inside your body that makes these “doors” in your gut wall open or close. And there are certain environmental triggers that make your cells produce zonulin.
One of these “triggers” is gluten. Humans, it turns out, were never meant to eat this food. And for most of human history, we didn’t. But once humans stopped living a hunter-gatherer lifestyle and started farming, gluten became a staple of our diets. Which might not have been a problem, except for one thing.
You see, gluten has certain protein “fragments” that humans can’t digest. Because of that, these “fragments” communicate with the soldiers on your gut wall and say, “Please, release zonulin and let us in.” Your immune system, though, thinks these proteins are invaders and starts fighting back. This causes inflammation.
This inflammation is what leads to the condition millions of people around the globe suffer from—leaky gut. Leaky gut refers to a condition in which the lining of the GI tract becomes porous – allowing toxins and other harmful chemicals to “leak” through.
What are the long-term effects of celiac disease?
Untreated celiac disease can lead to many long-term health complications.
According to the Celiac Disease Foundation, people with Celiac Disease have a 2x greater risk of developing coronary artery disease and a 4x greater risk of developing small bowel cancers.
And Celiac Disease can also lead to other autoimmune diseases as well, including type 1 diabetes and multiple sclerosis (MS). This is partly because celiac disease can cause both leaky gut and widespread inflammation throughout the body.
Is there a cure for Celiac Disease?
According to most mainstream medical sources, celiac is a disease without a cure. However, according to Dr. Steven Gundry – a former cardiothoracic surgeon and best-selling author of The Plant Paradox and The Longevity Paradox – celiac disease and its symptoms are not only diminished in his practice, but often reversed and cured.
That’s because for many of Dr. Gundry’s celiac patients, gluten is just the tip of the iceberg. Roughly 70% of his celiac patients continue to have celiac disease even after following a strict gluten-free diet for a year or more. And according to Dr. Gundry, this is because most of the gluten-free foods they’re eating are loaded with another type of dangerous protein called lectins (like corn and soy), that act similarly in the gut to gluten.
“In my practice,” Dr. Gundry says, “seventy percent of people who are sensitive to gluten react to corn as if it was wheat! I have only one patient who remains celiac after two years, and she not only eats in restaurants, but her husband has toast every morning that she makes for him!”
By contrast, all of Dr. Gundry’s other celiac patients typically see their symptoms resolve in 6-9 months – often for good.
So if you or someone you know has celiac disease, here is just one immediate step you must take to diminish the debilitating symptoms of celiac: You must stop eating gluten immediately. This means cutting the following foods out of your diet:
- Pasta
- Noodles
- Breads and pastries
- Crackers
- Cereal and granola
- Baked goods
- Beer
Ingesting even small amounts of gluten – in the form of foods contaminated with gluten or even crumbs – can lead to triggering of symptoms. So be sure to double-check the labels of any packaged foods and, if eating out, check with the restaurant to make sure your meal doesn’t contain any traces of gluten.
Additionally, gluten can “hide” in many surprising places, including:
- Medication and supplements
- Meat, fish, and poultry products
- Meat substitutes
- Oats
- Gluten-free frozen foods (like pizza)
- Restaurant food (even if it says it’s gluten-free)
- Beverages and alcohol
For those with celiac disease, it’s often essential to stay on a gluten-free diet for the rest of your life. While difficult, following a gluten-free diet has never been easier than it is today, with countless alternatives available at most grocery stores.
Once you’ve cut gluten from your diet, you will likely experience a reduction in symptoms within a few days. Over time, your small intestine will heal, and your villi will return to normal function.
Get your own personalized Celiac Disease care and recommendations from Dr. Gundry-approved care coordinators
If you do suspect you may have Celiac Disease, or if you’re already suffering from Celiac Disease, there are some steps you can take right at home.
Former heart surgeon and New York Times bestselling author Dr. Steven Gundry always begins with blood work. He looks for specific markers of autoimmune disease and other key indicators of a bigger problem (like markers for gluten sensitivity).
Next, Dr. Gundry has his Celiac patients begin his specific dietary program. While this includes cutting gluten from the diet, it also includes cutting other inflammatory foods like sugar and especially lectins. However, this is not an elimination diet, nor is it about depriving yourself or feeling hungry.
If you’re looking for more guidance than these simple recommendations for Celiac Disease, Dr. Gundry’s unique health program is now available to you (without needing an appointment at one of Dr. Gundry’s two, waitlist-only West Coast clinics).
Thanks to the pioneering work of Dr. Gundry and his team at Gundry Health, care coordinators trained in Dr. Gundry’s unique holistic methods are now available to help you craft your own personalized Celiac Disease program.