Unraveling Relapsing Polychondritis: Gundry Health’s Innovative Approach to Autoimmune Disease Management
Relapsing polychondritis (RP) is a rare disorder characterized by recurrent inflammation and destruction of cartilage and other connective tissues in the body. Cartilage is a tough, flexible tissue found in the ears, nose, joints, and other areas of the body.
RP is considered an autoimmune disease, which means that the body’s immune system, which is supposed to protect against foreign invaders, mistakenly attacks its own healthy tissues. In RP, the target is primarily cartilage, leading to a range of symptoms and complications.
The prevalence of RP is not definitively known due to its rarity, but it’s estimated to affect about 3.5 in one million people annually.
Symptoms
Relapsing polychondritis (RP) is characterized by a wide range of symptoms that result from recurrent inflammation and destruction of cartilage and other connective tissues in the body. The severity and specific symptoms can vary among individuals, but common symptoms of RP include:
- Pain and Tenderness: Individuals with RP often experience pain and tenderness in the affected areas. This can include the ears, nose, joints, and sometimes the chest or ribs.
- Swelling and Redness: Inflammation of the cartilage can lead to swelling and redness, particularly in the ears and nose. This can cause the ears to appear larger or misshapen.
- Respiratory Symptoms: RP can affect the airways, including the trachea and bronchi. This can lead to respiratory symptoms such as coughing, difficulty breathing, wheezing, and a sensation of tightness in the chest.
- Joint Pain: Some individuals with RP experience joint pain and inflammation, similar to symptoms of arthritis. Joint involvement can lead to stiffness and reduced range of motion.
- Eye Inflammation: Inflammation of the eyes, known as episcleritis or scleritis, can occur in RP. This can cause redness, pain, and sensitivity to light.
- Skin Problems: Skin issues may arise, including rashes, hives, or ulcerations.
- Heart and Blood Vessel Involvement: RP can affect the heart and blood vessels, potentially leading to complications such as aortic aneurysms or inflammation of the heart lining (pericarditis).
- Neurological Symptoms: In rare cases, RP may affect the nervous system, leading to symptoms like headaches, hearing loss, or problems with balance.
- Fever and Fatigue: During disease flares, individuals with RP may experience fever, fatigue, and a general sense of unwellness.
Other Symptoms:
RP can affect various other parts of the body, resulting in symptoms such as gastrointestinal problems, kidney involvement, and even damage to the larynx and vocal cords.
It’s important to note that RP is a relapsing-remitting condition, meaning that symptoms come and go in episodes or flares. During remission periods, symptoms may improve or temporarily disappear. However, RP is a chronic condition, and over time, recurrent episodes of inflammation can lead to permanent damage of cartilage and surrounding tissues.
Diagnosis
Diagnosing RP can be challenging due to its rarity and the diversity of symptoms. Because the inflammation comes and goes, and the symptoms are not exclusive to RP, diagnosing RP can be challenging. Often the initial symptoms involve the ears or nose with redness and pain, and are thought to be due to an infection leading to treatment with antibiotics. And because the condition may spontaneously improve, the prescribed antibiotics might be assumed to have been effective.
Diagnosis typically involves a combination of clinical evaluation, medical history, imaging studies, and blood tests. Diagnosis of RP is established when a doctor observes at least three of the following symptoms developing over time: inflammation of both outer ears, painful swelling in several joints, inflammation of the cartilage in the nose, and inflammation of the eye. Although blood test results can help doctors diagnose RP, they alone cannot confirm a definite diagnosis of RP because sometimes the abnormalities they detect are present in healthy people or in people who have other disorders
Early diagnosis and appropriate treatment are crucial to manage symptoms, prevent complications, and improve the overall quality of life for individuals with RP.
Treating RP with Gundry Health’s Clinical Care Program
Gundry Health offers an innovative clinical care program designed to help manage autoimmune diseases like RP. Some key features of this program include:
- Expert Knowledge: Our team comprises experienced healthcare professionals who specialize in autoimmune diseases.
- Annual Labs: We offer up to four labs annually at no extra charge to help monitor your health status.
- Food Logging and Yes-No Food Lists: These features within our mobile app and desktop dashboard enable patients to keep track of their diet and identify potential triggers.
Leaky Gut
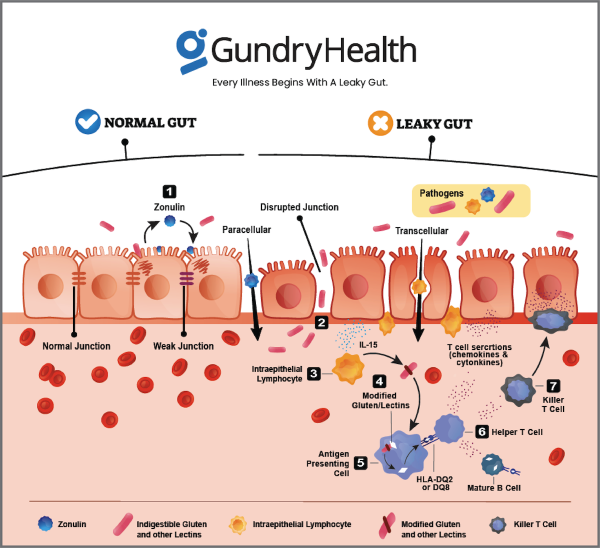
Relapsing Polychondritis is an autoimmune disease and one of the primary factors contributing to the development of autoimmune conditions is intestinal permeability, often referred to as “leaky gut.”
To comprehend the scientific intricacies of how leaky gut operates, it is essential to gain insight into the functioning of your gut wall. Your intestines are lined with a single layer of mucosal cells known as enterocytes. These cells are tightly interlocked to create a barrier that prevents the passage of substances in and out. Remarkably, despite being only one cell thick, this intestinal layer boasts a surface area equivalent to that of a tennis court.
Positioned along and interspersed within this lining are immune cells, specialized white blood cells that play a pivotal role in upholding the integrity of the gut wall. In fact, approximately 70-80 percent of all your immune cells are concentrated along the lining of your gut. These immune cells are responsible for determining what can exit the gastrointestinal tract and what must remain contained within.
The process of digestion begins with stomach acids, enzymes, and beneficial gut bacteria breaking down the food you consume into individual components: amino acids, fatty acids, and sugar molecules. Subsequently, your mucosal cells selectively absorb single molecules of these digested substances, transporting them through the cell’s interior and releasing them into either your portal vein or lymphatic system.
Under optimal conditions, everything except these single molecules of digested amino acids, fatty acids, and sugars remains outside the intestinal barrier, where it rightfully belongs. When the mucosal cells are tightly aligned, the gut lining effectively prevents the passage of other substances.
However, when the integrity of your gut wall becomes compromised, giving rise to microscopic openings, it permits the passage of additional compounds—a phenomenon known as “leaky gut syndrome” or intestinal permeability.
When inappropriate molecules or even bacteria breach the boundaries of your gut wall, your immune system springs into action. Ordinarily, this immune response is crucial as it can mobilize “reinforcements” in the form of inflammatory hormones called cytokines. Cytokines can be life-saving in cases of bacterial infection and assist in the healing process after injuries.
The issue arises when your immune system becomes hyperactive and responds to even minor triggers, such as environmental factors or food allergies. Think of it like an overly sensitive security alarm system: while it’s invaluable when it detects a genuine threat, it can become a nuisance when it goes off at the slightest disturbance, akin to a fly entering your home.
This is precisely what occurs in the context of a leaky gut. Your immune system starts reacting to virtually everything that breaches your porous gut wall, leading to a state of chronic inflammation.
Getting Rid of Autoimmune Disease and Leaky Gut With Lectin Free Diet
The idea of adopting a lectin-free diet has gained significant popularity in recent years. Dr. Steven Gundry, a California-based heart surgeon known for pioneering the lectin-free diet, suggests that lectins disrupt cell communication and promote inflammation. This disruption can lead to compromised gut health, resulting in a range of issues such as digestive problems (including bloating, gas, and diarrhea), weight gain, and a potential contribution to conditions like autoimmune diseases, obesity, and leaky gut syndrome.
Researchers now propose that eliminating lectins from your diet can offer numerous health benefits, including weight loss, the prevention of autoimmune conditions, improved overall health, and relief from various health problems.
So, what exactly are lectins?
Lectins are proteins that serve as a defense mechanism for plants. These proteins have the ability to bind carbohydrates (such as sugars, starches, and fibers), causing them to clump together and even attach to specific cells in your body when consumed.
Your gastrointestinal (GI) tract struggles to break down lectins effectively, which can lead to impaired digestion, reduced nutrient absorption, heightened immune system activation, and disturbances in your gut microbiome (the community of bacteria residing in your gut).
Furthermore, lectins have the potential to create a leaky gut by puncturing holes in your intestinal walls, allowing harmful bacteria and viruses to leak into your bloodstream. This can result in widespread inflammation, the type that can contribute to various autoimmune diseases.
How can you steer clear of lectins?
Common foods containing lectins include certain vegetables from the nightshade family (such as tomatoes, peppers, potatoes, and eggplants), squash, some fruits (though limited amounts of in-season fruits are typically allowed in the diet), grains, specific nuts and seeds like cashews and peanuts, as well as beans and legumes. Pressure-cooking certain foods can help reduce lectin content.
On the flip side, the following foods are known to have low lectin levels:
Pasture-raised meats
A2 milk
Cooked sweet potatoes
Leafy green vegetables
Cruciferous vegetables like broccoli and Brussels sprouts
Asparagus
Garlic
Onion
Celery
Mushrooms
Avocado
Olives or extra virgin olive oil
(You can find a complete Dr. Gundry YES/No food list HERE.)
Drawing from his two decades of experience in treating autoimmune diseases, Dr. Gundry has assisted numerous individuals, including many well-known celebrities. His Gundry Health program extends his expertise to a broader audience, making it accessible to those dealing with autoimmune conditions without the need for appointments at his exclusive West Coast clinics.
Thanks to Dr. Gundry and his team at Gundry Health, doctors trained in his holistic methods are now available to offer personalized guidance based on your unique health needs and goals. Each doctor at Gundry Health is Board Certified and proficient in Dr. Gundry’s renowned approach to functional medicine and healthcare.
Patient Experiences with Gundry Health
Many patients with RP have found Gundry Health’s clinical care program immensely helpful. For instance, Joane, a long-time sufferer of RP, reported significant improvements in her symptoms after participating in our program. She particularly appreciated the food logging feature, which helped her identify dietary triggers and adjust her eating habits accordingly.
Real-life patient experiences
Living with RP can be challenging due to the rarity of the disease and the lack of resources and information available for RP. Patients with RP may experience pain, tenderness, and swelling of the cartilage, which can lead to deformity and poor functioning1. Patients may also experience constitutional symptoms, including fatigue and flu-like symptoms8. However, there are support groups and patient organizations available to help patients connect with others who have RP and to provide resources and information about the disease910.
Taking Control of Your Health with Gundry Health
Managing an autoimmune disease like RP requires active participation and a comprehensive understanding of the condition. At Gundry Health, we’re committed to providing the tools and resources you need to take control of your health.
Whether you’re newly diagnosed with RP or have been managing it for years, Gundry Health’s clinical care program can provide the support you need. Visit our website to learn more about our services and how to get started on your journey to better health. Remember, you’re not alone in this fight, and with Gundry Health, you’re always in good hands.
In conclusion, RP is a rare autoimmune disease that causes inflammation of the cartilage in the body. The cause of RP is unknown, and diagnosing RP can be challenging due to the non-specific symptoms. Treatment for RP typically focuses on addressing symptoms and slowing the progression of the condition. Patients with RP may experience pain, tenderness, and swelling of the cartilage, which can lead to deformity and poor functioning. However, there are support groups and patient organizations available to help patients connect with others who have RP and to provide resources and information about the disease.
Get personalized care and recommendations for Unraveling Relapsing Polychondritis from Dr Gundry-Approved program
If you’re looking for more guidance about Unraveling Relapsing Polychondritis disease than this short list of recommendations, Dr. Gundry’s unique health program is now available to you (without needing an appointment at one of Dr. Gundry’s two, waitlist-only West Coast clinics).
Thanks to the pioneering work of Dr. Gundry and his team at Gundry Health, patient care team trained in Dr. Gundry’s unique holistic methods are now available to help you craft your own personalized Unraveling Relapsing Polychondritis program.
It’s easy to get started.
Simply click the link below to get more information about personalized Unraveling Relapsing Polychondritis treatment plan options, so you can get expert analysis, diagnostic care, and a plan for tackling Unraveling Relapsing Polychondritis, arthritis, or other autoimmune diseases.
Each patient care team member at Gundry Health is Board Certified and trained in Dr. Gundry’s renowned approach to functional medicine and care.
Get your personal lab data and talk to a U.S. licensed doctor. Click Here.